Common Surgical Position and Appropriate Management
Common Surgical Position and Appropriate Management
Supine Position
Supine position is a position of lying on the back or with the palm of the hand facing upwards (Figure 3.1). It is the most common position for surgery, induction of anesthesia and air way management. In a supine patient, one or both arms may be abducted out to the side or adducted (tucked toward the centre) alongside the body (Figure 3.2). It is recommended that upper extremity abduction (the movement of a limb or part of the body away from the centre line of the body) be limited to less than 90 degrees to minimize the likelihood of brachial plexus injury. The hand and forearm are either supinated or kept in a neutral position with the palm toward the body to reduce external pressure on the ulnar nerve. When the arms are adducted (the movement of a part of the body towards the midline .), they are usually held alongside the body with a "draw sheet" that passes under the body and over the arm and is then tucked directly under the torso (not the mattress) to ensure that the arm remains properly placed next to the body.
Because the entire body is close to the level of the heart, hemodynamic reserve is best maintained. However, because compensatory mechanisms are blunted by anesthesia, even a few degrees of head-down (Trendelenburg) position or head up (reverse Trendelenburg) position are sufficient to cause significant cardiovascular changes.


The Trendelenburg Position
tilting a supine patient head down (Figure 3.3) is often used to increase venous return during hypotension and to improve exposure during abdominal surgery. Nonsliding mattresses are recommended to prevent the patient from sliding cephalad. Shoulder braces are not recommended because of considerable risk of compression injury to the brachial plexus. The Trendelenburg position has significant cardiovascular and respiratory consequences. The head-down position increases central venous, intracranial, and intraocular pressures. Prolonged head- down position can also lead to swelling of the face, conjunctiva, larynx, and tongue with an increased potential for postoperative upper airway obstruction. The cephalad movement of abdominal viscera against the diaphragm also decreases functional residual capacity and pulmonary compliance. In spontaneously ventilating patients the work of breathing increases. In mechanically ventilated patients, airway pressures must be higher to ensure adequate ventilation. The stomach also lies above the glottis. Therefore, endotracheal intubation is often preferred to protect the airway from pulmonary aspiration of gastric contents and to reduce atelectasis. Because of the risk of edema to the trachea and mucosa surrounding the airway during surgeries in which patients have been in the Trendelenburg position for prolonged periods of time, an air leak should be verified around the endotracheal tube or the larynx visualized prior to extubation.

Trendelenburg position (head tilted down) and reverse Trendelenburg position (head tilted up).Shoulder braces should be avoided to prevent brachial plexus compression injuries
The Reverse
Trendelenburg position, supine with the head tilted upward, is often employed to facilitate upper abdominal surgery by shifting the abdominal contents caudad. Again, patients must be prevented from slipping on the table, and more frequent monitoring of arterial blood pressure may be prudent to detect hypotension due to decreased venous return. In addition, the position of the head above the heart reduces perfusion pressure to the brain and should be taken into consideration when determining optimal blood pressure.
Complications
Pressure alopecia, a condition in which hair is lost, due to ischemic hair follicles is related to prolonged immobilization of the head with its full weight falling on a limited area, usually the occiput. Hypothermia and hypotension during surgery may increase the incidence of this complication. Consequently, it is prudent to cushion the head well, during prolonged surgery, periodic rotation of the head to redistribute the weight may be considered.
Backache may occur in the supine position as the normal lumbar lordotic curvature; particularly the tone of the paraspinous musculature is lost during general anesthesia with muscle relaxation or a neuraxial block. Tissues overlying all bony prominences, such as the heels and sacrum, must be padded to prevent soft tissue ischemia due to pressure, especially during prolonged surgery.
Peripheral nerve injury remains a serious perioperative complication with a multifactorial etiology. Injuries occur when peripheral nerves are subjected to compression, stretch, ischemia, metabolic derangement, and direct trauma/laceration during surgery. Because sensation is blocked by unconsciousness or regional anesthesia, early warning symptoms of pain with normal spontaneous repositioning are absent. Ulnar neuropathy and brachial nerve injury is the most common lesion. Although there is no direct evidence that positioning or padding alone can prevent perioperative ulnar neuropathies, it is recommended to limit arm abduction in the supine patient to less than 90 degrees at the shoulder with the hand and forearm either supinated or kept in a neutral position. Regardless of the position of the upper extremities, maintaining the head in a relatively midline position can help minimize the risk of stretch injury to the brachial plexus.
Lithotomy Position
Lithotomy position is a position for surgical procedures (gynecologic, rectal, and urologic surgeries) or medical examinations in which the hips are flexed 80 to 100 degrees from the trunk and the legs are abducted 30 to 45 degrees from the midline (Figure 3.4). The knees are flexed until the lower legs are parallel to the torso, and the legs are held by supports or stirrups.
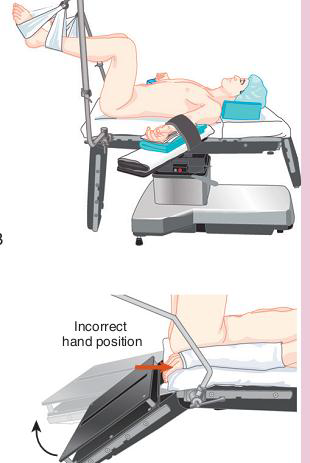
Positioning the arms on armrests far from the table hinge point is recommended at all times when patients are in lithotomy position to avoid a potentially disastrous crush injury to the fingers.
Initiation of the lithotomy position requires coordinated positioning of the lower extremities by two assistants to avoid torsion of the lumbar spine. Both legs should be raised together, flexing the hips and knees simultaneously. The lower extremities should be padded to prevent compression against the stirrups. Following the surgery, the patient must also be returned to the supine position in a coordinated manner. The legs should be removed from the holders simultaneously, knees brought together in the midline, and the legs slowly straightened and lowered onto the operating room table.
When the legs are elevated, preload increases, causing a transient increase in cardiac output and, to a lesser extent, cerebral venous and intracranial pressure in otherwise healthy patients. In addition, the lithotomy position causes the abdominal viscera to displace the diaphragm cephalad, reducing lung compliance and potentially resulting in a decreased tidal volume. If the patient is obese or a large abdominal mass is present (tumor, gravid uterus), abdominal pressure may increase significantly enough to obstruct venous return to the heart. Lastly, the normal lordotic curvature of the lumbar spine is lost in the lithotomy position, potentially aggravating any previous lower back pain. Patients undergoing surgery in the lithotomy position include injury to the common peroneal nerve caused by the compression of the nerve between the lateral head of the fibula and the bar holding the legs. The injury is more common with patients who had low body mass index and prolonged duration of surgery.
The Lateral Decubitus Position
Is most frequently used for surgery involving the thorax, retroperitoneal structures, or hip. The patient rests upon the nonoperative side and is balanced with anterior and posterior support such as bedding rolls or a deflatable beanbag, as well as a somewhat flexed dependent leg. The arms are usually positioned in front of the patient (Figure 3.5). The dependent (referring to a part of the body which is hanging down) arm rests upon a padded arm board perpendicular to the torso. The non dependent arm is often supported over folded bedding or suspended with an armrest or foam cradle. If possible, the arm should not be abducted more than 90 degrees.

The act of positioning a patient in the lateral decubitus position requires the cooperation of the entire operating room staff to prevent potential injuries. The patient's head must be kept in a neutral position to prevent excessive lateral rotation of the neck and stretch injuries to the brachial plexus.
The Prone or Ventral Decubitus Position
Lying face downwards (Figure 3.6), used primarily for surgical access to the posterior spine, the buttocks and perirectal area, and the lower extremities. As with the supine position, if the legs are in the same plane with the torso, hemodynamic reserve is relatively maintained, but if there is any significant lowering of the legs or tilt of the entire table, venous return may be decreased or augmented. Pulmonary function is not affected if there is no significant abdominal pressure and the patient is properly positioned.
The legs should be padded and flexed slightly at the knees and hips. The head may be supported face-down with its weight borne by the bony structures or turned to the side. Both arms may be positioned to the patient's sides, and tucked in the neutral position or placed next to the patient's head on arm board. Extra padding under the elbow will be needed to prevent compression of the ulnar nerve. Again, the arms should not be abducted greater than 90 degrees to prevent excessive stretching of the brachial plexus, especially in patients with the head turned.

When general anesthesia is planned, the trachea is first intubated while the patient is still on the stretcher, and all intravascular access is obtained as needed. The endotracheal tube is well secured to prevent dislodgment and loosening of tape due to drainage of saliva when prone. With the coordination of the entire operating room staff, the patient is then turned prone onto the operating room table, keeping the neck in line with the spine during the move. Blood pressure cuffs and other monitors should be disconnected before moving. Pulse oximetry can usually be maintained if applied to the "inside" arm, and complete monitoring should be reinstituted as rapidly as possible. Endotracheal tube position and adequate ventilation are reassessed immediately following the move.
Head position is critical. The patient's head may be turned to the side once prone if neck mobility is adequate. However, as in the lateral decubitus position, the dependent eye must be checked frequently for external compression. The face should be rechecked if any patient motion occurs during surgery, or if the table is significantly repositioned. The prone position is a risk factor for perioperative visual loss. Make sure pillows are used on the chest and pelvies to minimize ventilation compromise. Pad all dependant areas.