Ventilation
Ventilation
The adequacy of ventilation must be continuously evaluated throughout the course of an anesthetic.
Qualitative Methods of Evaluation
The simplest is observation of chest excursion or change in volume of the reservoir breathing bag of the anesthesia circuit during the ventilator cycle.
Auscultation of Breath sounds is also effective and is easily performed with precordial stethoscope, a heavily weighted bell applied to the chest over pericardium or sternal notch. Esophageal stethoscopes (Figure 2.2 and Figure 2.3) may be employed during general anesthesia whenever an endotracheal tube is used. Esophageal stethoscopes are available commercially and can be created with common materials such as stethoscope with a removable bell, suture, nasogastric tube and glove (Figure 2.3). These devices allow you to continually listen to and assess the patient's heart rate and lung sounds. It can alert you to problems such as light anesthesia, accidental extubation, need for suctioning secretions, accidental advancement of the endotracheal tube, and cardiac arrest. This form of monitoring should be used for all anesthetic cases. Breath sounds are auscultated via monaural ear piece, which also allows the anesthetist a free ear to communicate with OR personnel.


If the patient is breathing spontaneously you should continuously monitor your patient's respiration (Table2.3). Record the respiratory rate every 5 minutes.
Table 2.3 Normal Respiratory Rate at Different Age
| Age | Normal Respiratory Rate / Minute |
|---|---|
| Adult | 12- 20 breath |
| Children 1-8 years | 15 -30 breath |
| Infant 1- 12 months | 25- 50 breath |
| Neonate 1 - 28 days | 40-60 breath |
The quality of the patient's respirations can help guide you.
- Normal: may not need to be assisted with ventilation and may be at an adequate depth of anesthesia.
- Shallow: may require assistance with ventilation. May indicate that the patient is "too deep" therefore concentration of anesthetic may need to be decreased.
- Labored: may indicate that anesthesia is light therefore patient may require additional anesthetic/analgesics.
Quantitative Methods of Evaluation
SpirometerThe volume of gas exhaled by the patient can be measured by a spirometer placed in the expiratory limb placed in the expiratory limb of a circle breathing system. This devices permits a fairly accurate assessment of tidal volume (the volume of air which is inspired or expired per breath, 7-10 ml/kg) and minute ventilation.
Capnography is the monitoring of the concentration or partial pressure of carbon dioxide in the respiratory gases (Figure 2.4). The use of capnography has improved the margin of safety for patients undergoing general anesthesia.
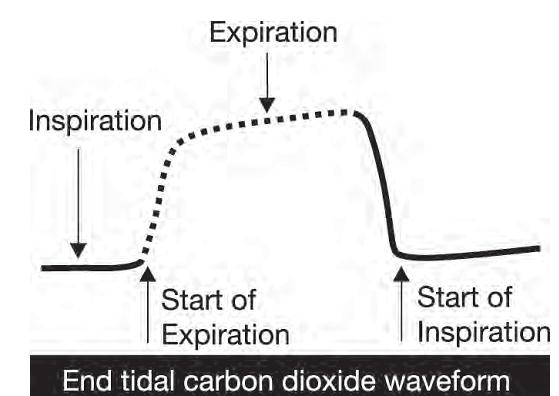
The normal range for end tidal carbon dioxide (ETCO2) is 35-45 mm Hg. Capnography is especially useful to identify the correct placement of an endotracheal tube in the trachea. If the endotracheal tube is placed in the esophagus there will be no end tidal carbon dioxide, or there will be four or less gradually declining waveforms (See ANNEX 1).