Methods of Maintenances of General Anesthesia
Methods of Maintenances of General Anesthesia
The Use of Inhalation Anesthetics for Maintenance of Anesthesia
The volatile anesthetics (e.g., halothane 0.5 -2 vol%) are clearly the most popular drug used to maintain anesthesia in Ethiopia. The continued popularity of volatile anesthetics for maintenance of anesthesia is due primarily to their rapid reversibility and ease of administration for titrating to the desired end point. They are easily administered via inhalation (through mask or endotracheal tube), they are readily titrated (the process of gradually adjusting the dose of medications until optimal results are reached), they have a high safety ratio in terms of preventing recall, and the depth of anesthesia can be quickly adjusted in a predictable way while monitoring tissue levels via end-tidal concentrations. They are effective regardless of age or body habitus. They have some properties that prove beneficial in maintenance of anesthesia; including relaxation of skeletal muscle (Volatile agents decrease nondepolarizer dosage requirements by at least 15 %.), in most cases preservation of cardiac output and cerebral blood flow, and relatively predictable recovery profiles. Some of the draw backs to the use of the current volatile anesthetics are the absence of analgesic effects, their association with postoperative nausea and vomiting. Muscle relaxants can be administered along with inhalation anesthetics dictated by surgical requirement.
Use of Intravenous Drugs for Maintenance of Anesthesia
Various different agents have been employed for intravenous techniques. Thiopentone was widely used in the 1950s and 1960s for continuous IV anesthesia but its accumulation in the tissues and, hence, prolonged recovery phase proved disadvantageous. Ketamine has proved useful in the developing countries. After IV administration of 1-2 mg/kg consciousness returns in 10 to 15 minutes, profound analgesia and amnesia may be maintained by continuous intravenous infusion (1 to 2 mg/kg/h) or intermittent injections (0.25 to 0.5 mg/kg every 15 minutes). Titrate infusion according patient response. Propofol is currently popular in developed countries and is in common use for total intravenous anesthesia (TIVA). The usual induction dose of propofol is 1 - 2.5 mg/kg, when used for maintenance by infusion, the infusion usually started at 100 to 200 μg/kg/min with opioids and supplementary boluses of propofol may be needed to ensure adequate depth of anesthesia.
The availability of intravenous (IV) drugs with more rapid onset and shorter recovery profiles has facilitated the maintenance of anesthesia with continuous infusions of IV drugs, producing an anesthetic state name total intravenous anesthesia (TIVA) that compares favorably with the volatile anesthetics. The traditional intermittent bolus administration of IV drugs results in a "depth" of anesthesia (and analgesia) that oscillates above and below the desired level. The use of IV anesthetic techniques requires continuous titration of the drug infusion rate to the desired pharmacodynamic end point.
Because of rapid distribution and redistribution of the IV anesthetics, the high peak blood concentration after each bolus is followed by a rapid decrease, producing fluctuating drug levels in the blood and hence the brain. The magnitude of the drug level fluctuation is dependent on the size of the bolus dose and the frequency of its administration. Wide variation in the plasma drug concentrations (the amount of drug present in the plasma or blood) can result in hemodynamic and respiratory instability as a result of changes in the depth of anesthesia or sedation. By providing more stable blood (and brain) concentrations with a continuous IV infusion, it might be possible to improve anesthetic conditions and hemodynamic stability, as well as decreasing side effects and recovery times with IV anesthetics.
The required plasma concentration depends on the desired pharmacological effect (hypnosis, sedation), the concomitant use of other adjunctive drugs (opioid analgesics, muscle relaxants, cardiovascular drugs), the type of operation (superficial, intra-abdominal, intracranial), and the patient's sensitivity to the drug (age, drug history, preexisting diseases). Preexisting diseases (cirrhosis, congestive heart failure, renal failure) can markedly increase the toxicity level; children have higher clearance rates, while the elderly have reduced clearance values. Various intraoperative interventions (laryngoscopy, tracheal intubation, skin incision, entry into body cavities) transiently increase the anesthetic and/or analgesic requirements. Therefore, the infusion or alternate bolus scheme should be tailored to provide peak drug concentrations during the periods of most intense stimulation. It must be emphasized that the therapeutic window for Sedative-hypnotics is markedly influenced by the presence of analgesic drug (e.g., pethedine, fentanyl).
Assessing depth of IV anesthesia based on somatic and autonomic signs (changes in muscle tone, respiratory rate and pattern, autonomic hyperactivity such as tachycardia, hypertension, lacrimation, and diaphoresis in light anesthesia) are sensitive clinical signs of depth of anesthesia as well as titrating IV anesthetics. Unfortunately, the anesthetic drugs (ketamine), as well as adjunctive agents (α agonists, β blockers, adenosine, calcium-channel blockers), can directly influence the cardiovascular response to surgical stimulation.
Although the cardiovascular signs of autonomic nervous system hyperactivity may be masked, other autonomic signs (e.g., diaphoresis) and purposeful movements may be more reliable indicators of depth of anesthesia than blood pressure. The heart rate response to surgical stimulation appears to be more useful than the blood pressure response in determining the need for additional analgesic medication. Moreover, it would appear that blood pressure and heart rate responses to surgical stimulation are a less useful guide with IV techniques than with volatile anesthetics. The clinical assessment of anesthetic depth has become more challenging because IV anesthetic techniques involve a combination of hypnotics, opioids, muscle relaxants, and adjuvant drugs.
Maintenance of Relaxation
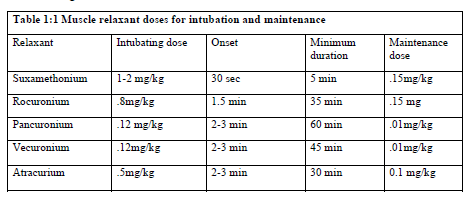
Following intubation, muscle paralysis may need to be continued to facilitate surgery, e.g., abdominal operations, or anesthetic management, e.g., hemodynamic compromise precluding deepening anesthesia or the need to control ventilation. The variability between patients in dose responses to muscle relaxants cannot be overemphasized. Maintenance doses (Table 1.1) whether by intermittent boluses or continuous infusion should be guided by the nerve stimulator and clinical signs (eg, spontaneous respiratory efforts or movement). In some instances clinical signs may precede nerve stimulator because of differing sensitivities to muscle relaxants between muscle groups or technical problems with the nerve stimulator. Some return of neuromuscular transmission should be evident prior to administering each maintenance dose.