Advanced Cardiac Life Support
Advanced Cardiac Life Support
Effective ACLS begins with high-quality BLS, particularly high-quality CPR. Changes in the ACLS treatment of cardiac arrest have been designed to minimize interruptions in chest compressions for rhythm check, pulse check, and ACLS therapies. To minimize interruptions in chest compressions, the resuscitation team leader should plan interventions such as rhythm checks, insertion of an airway, and even drugs administration around uninterrupted periods of CPR. The potential effects of any drugs or ACLS therapy on outcome from VF/ Sudden Cardiac Arrest are dwarfed by the potential effects of immediate, high-quality CPR and early defibrillation. There is much less emphasis on drug therapy during cardiac arrest and much more emphasis on CPR with minimal interruptions in chest compressions.
Major changes in ACLS include (2005 guideline)
- Emphasis on high-quality CPR. Particularly rescue breaths with chest compressions and emphasis on chest compression depth and rate, chest wall recoil, and minimal interruptions.
- Increased information about use of LMA and esophageal-tracheal combitube (Combitube). Use of endotracheal intubation is limited to providers with adequate training and opportunities to practice or perform intubations.
- Confirmation of endotracheal tube placement requires both clinical assessment and use of a device (eg,exhaled CO2 detector, esophageal detector device). Use of a device is part of (primary) confirmation and is not considered secondary confirmation.
- The algorithm for treatment of pulseless arrest was reorganized to include VF/pulseless VT, asystole, and PEA.
- The priority skills and interventions during cardiac arrest are BLS skills, including effective chest compressions with minimal interruptions.
- Insertion of an advanced airway may not be a high priority. If an advanced airway is inserted, rescuers should no longer deliver cycles of CPR. Chest compressions should be delivered continuously (100 per minute) and rescue breaths delivered at a rate of 8 to 10 breaths per minute (1 breath every 6 to 8 seconds).
- Providers must organize care to minimize interruptions in chest compressions for rhythm check, shock delivery, advanced airway insertion, or vascular access.
- Intravenous or intraosseous (IO) drug administration is preferred to endotracheal administration.
- Treatment of VF/pulseless VT: To attempt defibrillation, 1 shock is delivered using monophasic or biphasic waveforms followed immediately by CPR (beginning with chest compressions).
- Rescuers should minimize interruptions in chest compressions and particularly minimize the time between compression and shock delivery, and shock delivery and resumption of compressions.
- Compressions should ideally be interrupted only for rhythm checks and shock delivery. Rescuers should provide compressions (if possible) after the rhythm check, while the defibrillator is charging. Then compressions should be briefly interrupted when it is necessary
- clear the patient and deliver the shock, but the chest compressions should resume immediately after the shock delivery.
- Providers do not attempt to palpate a pulse or check the rhythm aftershock delivery.
- If an organized rhythm is apparent during rhythm check after 5 cycles (about 2 minutes) of CPR, the provider checks a pulse.
- Drugs should be delivered during CPR, as soon as possible after rhythm checks. If a third rescuer is available, that rescuer should prepare drug doses before they are needed.
- If a rhythm check shows persistent VF/VT, the appropriate vasopressor or antiarrhythmic should be administered as soon as possible after the rhythm check. It can be administered during the CPR that precedes (until the defibrillator is charged) or follows the shock delivery.
- The timing of drug delivery is less important than is the need to minimize interruptions in chest compressions.
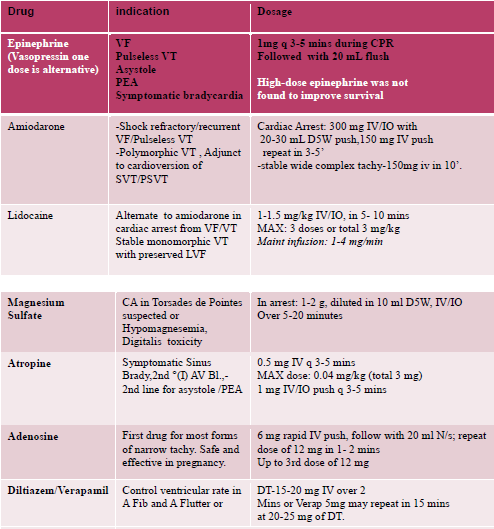
- Vasopressors are administered when an IV/IO line is in place, typically if VF or pulseless VT persists after the first or second shock. Epinephrine may be given every 3 to 5 minutes. A single dose of vasopressin may be given to replace either the first or second dose of epinephrine.
- Antiarrhythmics may be considered after the first dose of vasopressors(typically if VF or pulseless VT persists after the second or third shock). Amiodarone is preferred to lidocaine, but either is acceptable.
- Treatment of asystole/pulseless electrical activity: epinephrine may be administered every 3 to 5 minutes. One dose of vasopressin may replace either the first or the second dose of epinephrine.
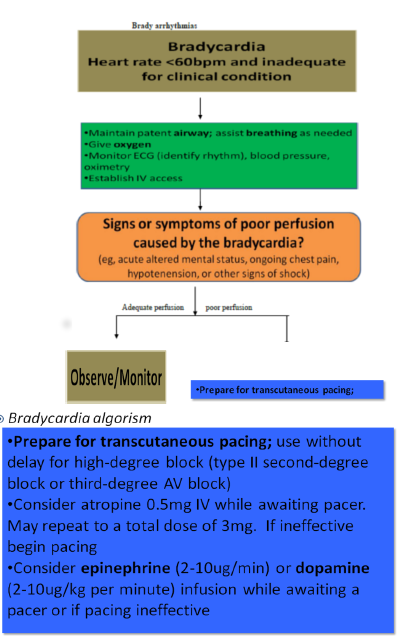
- Treatment of symptomatic bradycardia: the recommended atropine dose is now 0.5 mg IV, may repeat to a total of 3mg. Epinephrine or dopamine may be administered while awaiting a pacemaker.
- Treatment of symptomatic tachycardia: a single simplified algorithm includes some but not all drugs that may be administered. The algorithm indicates therapies intended for use in the in-hospital setting with expert consultation available.
- Post resuscitation stabilization requires support of vital organs, with the anticipation of post resuscitation myocardial dysfunction.
- Avoid hyperthermia for all patients after resuscitation. Consider inducing hypothermia if the patient is unresponsive but with an adequate blood pressure following resuscitation.
SCD (Sudden Cardiac Death)
- SCD-death due to cardiac causes heralded by abrupt loss of consciousness in an individual with/without known preexisting heart disease.
- CA (cardiac arrest)-Abrupt cessation of cardiac pump function which may be reversed by prompt intervention.
- Cardiovascular collapse-acute loss of effective blood flow to distal organs.
Etiologies of SCD
Structural
- coronary artery disease
- myocardial hypertrophy
- dilated cardiomyopathy
- valvular heart disease
- electrophysiological abnormalities
Functional
- electrolyte abnormalities, hypoxia, acidosis
- Mostly the causes of SCD are Ventricular fibrillation/tachycardia, Pulsels Electrical Activity, and asystole
Ventricular Fibrillation and Pulseless VT:
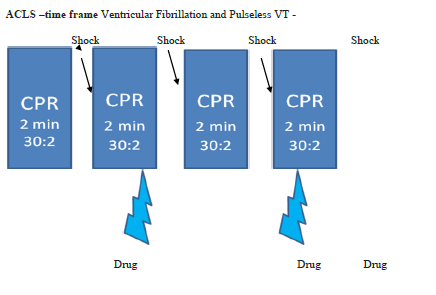
- This illustrates suggested timing of CPR, rhythm checks, attempted defibrillation (shock delivery), and drug delivery for persistent VF/ pulseless VT.
- Drug doses should be prepared prior to rhythm check. Drugs should be administered during CPR, as soon after a rhythm check as possible.
- Ideally CPR (particularly chest compressions) is interrupted only for rhythm check and shock delivery. If possible, rescuers should perform chest compressions while the defibrillator is charging.
- Rescuers should resume chest compressions immediately after a shock is delivered.
- In in-hospital settings with continuous (eg, electrocardiographic, hemodynamic) monitoring in place, this sequence may be modified by the physician.
- If PEA or asystole develops after a shock (and CPR), rescuers should follow the Asystole/PEA branch of the ACLS or PALS Pulseless Arrest Algorithms.
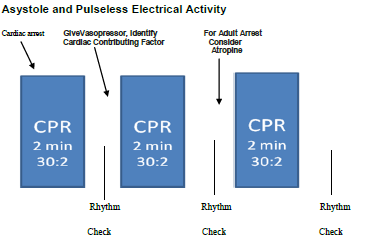
- Drug doses should be prepared prior to rhythm check. Drugs should be administered during CPR, as soon after a rhythm check as possible.
- Rescuers should search for and treat any contributing factors. Ideally CPR (particularly chest compressions) is interrupted only for rhythm check and shock delivery
- In in-hospital settings with continuous (eg, electrocardiographic, hemodynamic) monitoring in place, this sequence may be modified by the physician.
- If VF/pulseless VT develop, rescuers should follow the VF/Pulseless VT branch of the ACLS or PALS Pulseless Arrest Algorithm
- Identify contributing factors such as 5H(hypoxia ,hypovolemia, hypokalemia/hyperkalemia, hydorgen/acidosis ,hypothermia), and 5T(Toxins, tamponade, thromboembolism, Tension PT, trauma)
- Defibrillation not successful, Atropine is also questioned.
Post Cardiac Resuscitation Care
- Therapeutic hypothermia(32-34°C)
- Hemodynamic optimization(hypotension treatment)
- Ventilation optimization (Sao2≥94%)
- Immediate coronary reperfusion with PCI (percutaneous coronary intervention)
- Moderate glycemic control measures should be implemented to maintain glucose levels from 144-180 mg/dL to avoid hypoglycemia)
Atrrial Fibrillation
- Stable-Beta blockers, calcium channel blockers,amiodarone
- Unstable with hypotension and shock-cardioversion with 100-200J(there is risk of embolism)
Emergency Preperdiness
- Drugs-ready ,even in a syringe
- IV line, vigo
- Air way adjuncts ready
- Defibrillator charged
- Hard board for resucitation
- Team formulated
- Trainings and simulations
ACLS Team
- Team Leader - organizes the group, monitors individual performance of team members, models excellent team behavior, trains and coaches, facilitates understanding and focuses on comprehensive patient care.
- Team Member - must be proficient to perform skills within their scope of practice. They are clear about their role assignment
- Team Dynamics and Communication-Closed loop communication, Clear messages, Clear roles and responsibilities, Knowing one's limitations, Constructive intervention.