The Differences Between the Adult and Child
The Differences Between the Adult and Child
The differences between the adult and child can be classified as: anatomical, physiological, pharmacological, psychological and pathological
Anatomical Differences
Children are small and they require special equipment of the appropriate size (the neonate is one twentieth the size of the adult). Drugs and fluids are given according to the weight of the child. All children should be weighed prior to surgery but the following table may be used as a rough guide to weight in healthy children.
![]()
The surface area is large in relation to weight. This means the child loses heat more easily and loses more fluid from the skin. The veins may be difficult to cannulate.
The respiratory tract shows many differences and the child has limited respiratory reserve. Breathing in infants is relatively inefficient and takes a lot of the child's energy. Anything which makes the work of breathing harder will rapidly cause respiratory failure. Neonates and infants should be intubated and ventilated for all except brief surgical procedures. The infant's head and tongue are large and the airway is easily obstructed. The older child may have large tonsils and adenoids. Under anaesthesia a clear airway is maintained by lifting the chin, using jaw thrust and avoiding compression of the floor of the mouth. An oropharyngeal airway of the correct size may be useful. The larynx in the child is placed higher at (C3/C4) than in the adult (C5/C6). It is also more anterior. The epiglottis is large, floppy and is more easily seen using a straight blade laryngoscope, which lifts the epiglottis out of the way. This factor, together with limited respiratory reserve may make intubation difficult in infants. The narrowest part of the adult larynx is between the vocal cords. In the child it is lower down at the level of the cricoid cartilage. The implication of this is that the tube may pass quite easily between the cords but fit tightly at the level of the cricoid, resulting in laryngeal oedema post-operatively. Avoid using a tracheal tube which is too large. The trachea in children is relatively short and it is easy to put the tracheal tube down too far. The position of the tube should always be checked by listening with a stethoscope.
The airways are small and easily blocked by secretions. A clear nasal airway is especially important for small infants as they breathe predominantly through their noses while feeding. In infants the ribs are horizontal and elastic, the lungs are very compliant and distal airway collapse is common. The diaphragm is an important muscle of respiration - abdominal distension will splint the diaphragm and make respiration inefficient. A nasogastric tube should be passed to relieve abdominal distension. The apparatus dead space is relatively large compared with the small tidal volume of the child (7-10 ml/kg). Dead space and the resistance of the breathing circuit should be minimised to reduce the work of breathing.
The central nervous system. In the infant the spinal cord ends at the level of L3 (L1 in children > 1 year and adults). Lumbar punctures should be performed at the level of L5 / S1 in infants.
Physiological Differences
Energy Metabolism: The basal metabolic rate is higher in the child than the adult. The oxygen consumption in the neonate is 7ml/kg compared with 4 ml/kg in the adult. Infants rely on a rapid respiratory rate to provide adequate minute ventilation (resting respiratory rate is twice that of adults). Interruption of breathing for any reason results in rapid desaturation.
Respiratory System. The respiratory centre in newborns is immature and they are prone to stopping breathing (apnoeas) for the first few weeks of life, especially if they become hypoxic. Young infants are extremely sensitive to respiratory depressants (e.g.opioids).
The heart in infants is immature and sensitive to the depressant effects of anaesthetic agents. The cardiac output is high. The cardiac stroke volume is relatively fixed and cardiac output is maintained by a relatively high resting heart rate (at least 120 beats/min in infants). Bradycardia results in a rapid fall in cardiac output.
Vagal tone is well developed in infants and they are prone to reflex bradycardias (intubation, hypoxia, drugs). Atropine is useful as a premedication or should be readily available. The blood pressure in newborns is 60-90mmHg and increases with increasing sympathetic tone to reach adult levels by 10 years of age. In measuring BP in a child, it is important to use a cuff of the correct width for the arm or leg. It should be the largest size which will fit the limb.
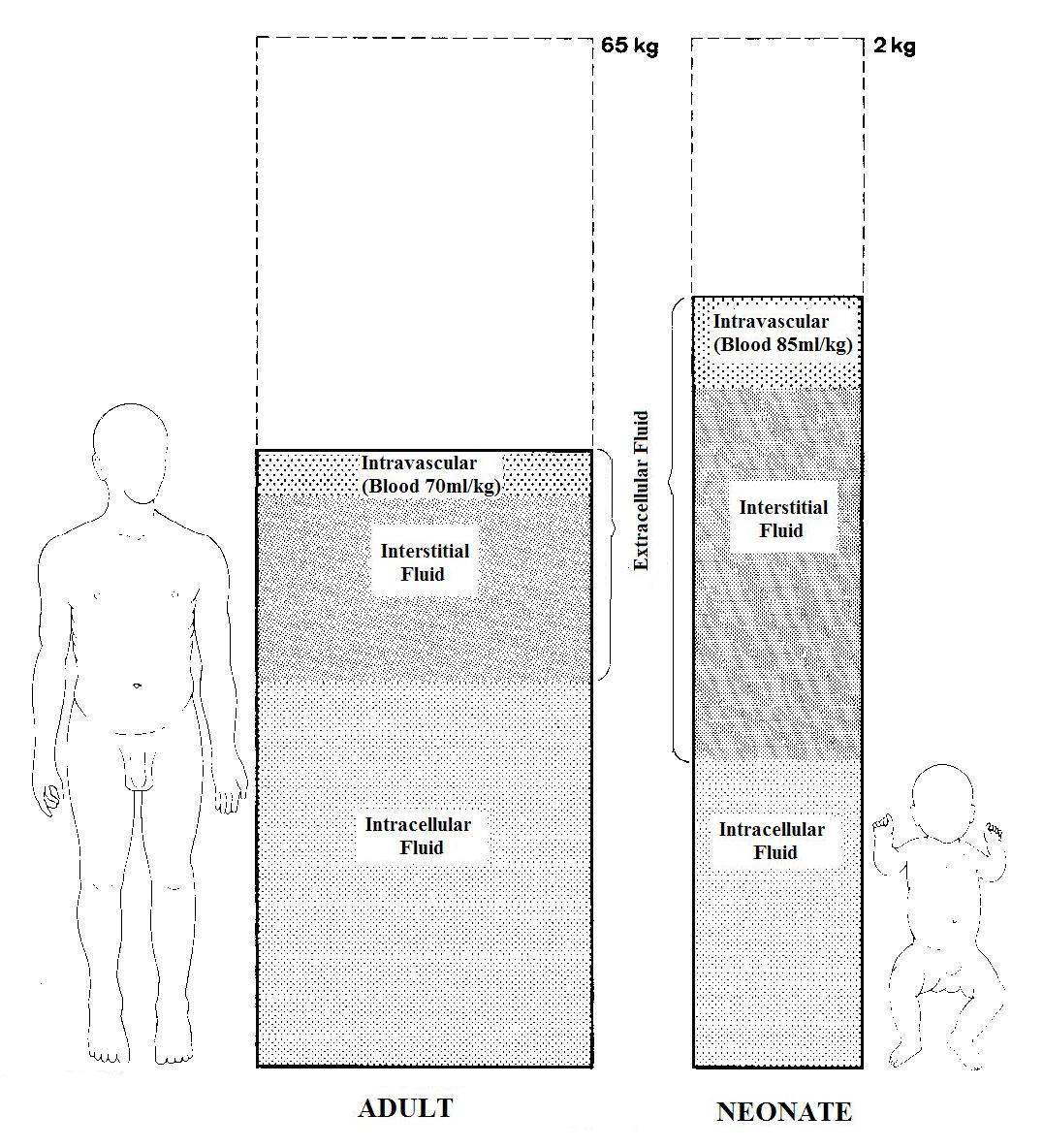
The blood volume, which is calculated on the basis of the body weight, may appear very small. For example: If a child weighing 25 kg has a tonsillectomy, then a loss of 200 ml would constitute 10% of total blood volume (25 kg x 80 ml = 2000 ml). If an adult lost 200ml of blood it would not be significant but a child losing that amount would need a transfusion.
Allowable blood loss may be small and will depend on the child's starting haemoglobin and the circulating blood volume. Blood transfusion should be considered when there is a 10-15% loss in blood volume. Circulating blood volume is calculated using the formula:
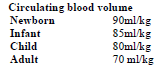
Fluids and Electrolytes
Isotonic solutions (Ringer's or 0.9% saline) should be used during surgery for all children. Neonates have limited glycogen stores and are prone to hypoglycaemia. Added dextrose (5% dextrose in Ringer’s or 0.9% saline) should be considered for neonates and other children requiring a dextrose infusion prior to surgery to maintain blood glucose. Children are prone to iatrogenic hyponatraemia, and postoperative fluids should be given as 0.45% saline or 0.9% saline with dextrose.
Renal function in infants is immature. They produce large volumes of dilute urine and can become dehydrated if fasted for prolonged periods of time. Conversely fluid requirements may be small in absolute terms and fluid overload should be avoided.
7.1.2.5 Temperature control.
Infants have immature thermoregulatory mechanisms and are prone to heat loss, especially under anaesthesia, due to vasodilatation and loss of shivering. The body temperature tends to follow that of the environment and active measures should be taken to minimise heat loss, at the same time avoiding hyperthermia. The dangers of hypothermia include clotting abnormalities, delayed drug metabolism (opioids, muscle relaxants), impaired wound healing and infection
Doses of Commonly Used Drugs (in Healthy Children)
| DRUG | DOSAGE | ROUTE | NOTES |
|---|---|---|---|
| Premedicants and Sedatives | |||
| Atropine | 10micrograms/kg 20micrograms/kg | IV IM | |
| Paracetamol | 20mgs/kg | Orally | |
| Trimeprazine | 2mgs/kg | Orally | |
| Midazolam | 0.5mg/kg | Orally | Give 20-30 mins pre-operatively. |
| Diazepam | 0.2mg/kg | IV | Not recommended if alternative available. |
| Induction Agents | |||
| Thiopentone | 5mg/kg | IV | |
| Propofol | 3-5mg/kg | IV | |
| Etomidate | 0.3mg/kg | IV | |
| Ketamine | 1-2mg 5-7mg | IV IM | |
| Relaxants | |||
| Suxamethonium | 2mg/kg (neonate) 1.5mg/kg (child) | IV IV | |
| Pancuronium | 0.1mg/kg | IV | 1/3 of initial dose can be given as an increment. |
| Atracurium | 0.5mg/kg | IV | |
| Vecuronium | 0.1mg/kg | IV | |
| Rocuronium | 0.6mg/kg | IV | |
| Reversal Agents | |||
| Atropine | 20 micrograms/kg | IV | |
| Glycopyrrolate | 50 micrograms/kg | IV | |
| Analgesics | |||
| Paracetamol | 20mgs/kg | Orally | Max. 90mgs/kg/day |
| Ibuprofen | 5-10mgs/kg | Orally | |
| Diclofenac | 1mg/kg | Rectally | |
| Fentanyl | 1-2 micrograms/kg | IV | |
| Glycopyrrolate | 10 micrograms/kg | IV | |
| Pethidine | 1mg/kg | IV or IM | |
| Morphine | 100 micrograms/kg | IV, IM or SC | |
| Pentazocine | 500 micrograms/kg 1mg/kg | IV IM or S | In children over one year. |
Pharmacological Differences
Both the actions and side effects of many drugs differ in children from adults. Doses are calculated on a weight basis.
The blood pressure of neonates and infants tends to be more sensitive to volatile anesthetics, probably because of not fully developed compensatory mechanisms (eg, vasoconstriction, tachycardia) and an immature myocardium that is very sensitive to myocardial depressants
Note that in the case of muscle relaxants the neonate has unusual requirements.
Suxamethonium: neonates and young infants are resistant to suxamethonium because of high volume of distribution and rarely show fasciculation and are more prone to bradycardia. Thus prepare atropine before administration of sux.to treat or prevent the effect of bradycardia.
Non-depolarising agents: neonates are very sensitive to non-depolarising drugs. In all children less than 5 years of age the risk of laryngeal spasm and bradycardia can be reduced by giving atropine 10 -20 micrograms/kg IM or IV either pre-operatively or at induction.
For older children a friendly and simple explanation along with the use of topical creams, if available, will often avoid the need for preoperative sedation.
Psychological Differences
There is difficulty in communication, especially in the first five years. Deprivation develops rapidly, especially after separation from the parents. There is a great fear of injections and a greater fear of the unknown in young children.
Pathological Differences
Children presenting for surgery are often very ill. There may be other associated congenital abnormalities, especially in the neonates.