Histamine Receptors
Histamine Receptors
Histamine is found in the central nervous system, in the gastric mucosa, and in other peripheral tissues. Histaminergic neurons are primarily located in the posterior hypothalamus but have wide projections in the brain. Histamine normally plays a major role in the secretion of hydrochloric acid by parietal cells in the stomach. The highest concentrations of histamine are found in the storage granules of circulating basophiles and mast cells throughout the body.
Types of Histamine Receptors
- H1 receptors: mediate effects on smooth muscle leading to vasodilation, increased vascular permeability, and contraction of nonvascular smooth muscle (e.g., bronchial muscle).
- H2 receptors: mediate histamine stimulation of gastric acid secretion and may be involved in cardiac stimulation.
- H3 receptors: feedback inhibitors in CNS, gastrointestinal tract, lung, heart.
Conditions That Release Histamine
- Tissue injury: Any physical or chemical agent that injures tissue, skin or mucosa is particularly sensitive to injury and will cause the immediate release of histamine from mast cells.
- Allergic reactions: exposure of an antigen to a previously sensitized (exposed) subject can immediately trigger allergic reactions.
- Drugs and other foreign compounds: morphine, dextran, antimalarial drugs, dyes, antibiotic bases, alkaloids, amides, Toxins and venoms.
Mechanism of Action and Clinical Uses
H 1 receptor antagonist mechanism of action: diphenhydramine is an example of a diverse group of drugs that competitively blocks h1-receptors. Many drugs with h1-receptor antagonist properties have considerable atropine-like; activity (e.g., dry mouth) and antiemetic (prevent vomiting)
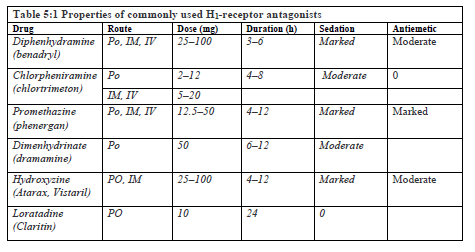
Clinical Uses: Diphenhydramine has a multitude of therapeutic uses (Table 5.1): suppression of allergic symptoms (e.g., urticaria, rhinitis, conjunctivitis); vertigo, nausea, and vomiting (e.g., motion sickness); sedation and suppression of cough. Although H1-blockers prevent the bronchoconstrictive response to histamine, they are ineffective in treating bronchial asthma. Likewise, H1-blockers will not completely prevent the hypotensive effect of histamine. Thus, the usefulness of H1-blockers during an acute anaphylactic reaction is quite limited; epinephrine is the treatment of choice. The antiemetic and mild hypnotic effects of antihistaminic drugs (particularly diphenhydramine, promethazine, and hydroxyzine) have led to their use for premedication. Although many H1-blockers cause significant sedation, ventilatory drive is usually unaffected in the absence of other sedative medications. Promethazine and hydroxyzine are often combined with opioids to potentiate analgesia. Newer (second-generation) antihistamine e.g., loratadine tend to produce little or no sedation because of limited penetration across the blood-brain barrier. This group of drugs is available only in oral preparations that are used primarily for allergic rhinitis and urticaria.
Drug interactions: The sedative effects of H1-receptor antagonists can potentiate other central nervous system depressants such as barbiturates, benzodiazepines, and opioids.
H2-receptor antagonist mechanism of action: include cimetidine, famotidine, and ranitidine. These agents competitively inhibit histamine binding to H2-receptors, thereby reducing gastric acid output and raising gastric pH.
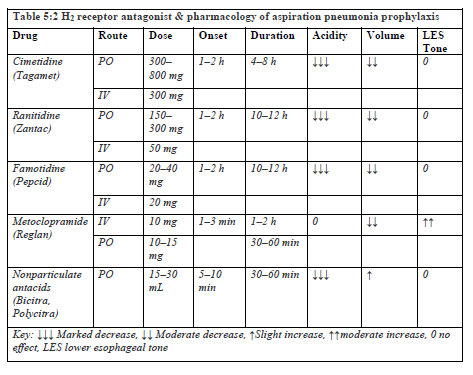
Clinical uses: All H2-receptor antagonists are effective in the treatment of peptic duodenal and gastric ulcers, hypersecretory states, and gastro esophageal reflux disease (GERD). Intravenous preparations are also used to prevent stress ulceration in critically ill patients. Duodenal and gastric ulcers are usually associated with Helicobacter pylori infection, which is also treated with combinations of bismuth, tetracycline, and metronidazole. Ranitidine bismuth citrate with clarithromycin may also be used for peptic ulcers associated with H pylori infection. By decreasing gastric fluid volume and hydrogen ion content, H2-blockers reduce the perioperative risk of aspiration pneumonia (Table 5.2). These drugs affect the pH of only those gastric secretions that occur after their administration.
Side Effects: Rapid intravenous injection of cimetidine and ranitidine has been rarely associated with hypotension, bradycardia, arrhythmias, and cardiac arrest. These adverse cardiovascular effects are more frequent following the administration of cimetidine to critically ill patients. In contrast, famotidine can be safely injected intravenously over a 2-min period. H2-Receptor antagonists change the gastric flora by virtue of their pH effects. Complications of long-term cimetidine therapy include hepatotoxicity (elevated serum transaminases), interstitial nephritis (elevated serum creatinine), granulocytopenia, and thrombocytopenia.
Drug interactions: Cimetidine may reduce hepatic blood flow and binds to the cytochrome P-450 system. These effects slow the metabolism of a multitude of drugs, including lidocaine, Propranolol, diazepam, theophylline, Phenobarbital, warfarin, and phenytoin. Ranitidine is a weak inhibitor of the cytochrome P-450 system, and no significant drug interactions have been demonstrated. Famotidine do not appear to affect the cytochrome P-450 system.