Physiology of Respiratory System
Physiology of Respiratory System
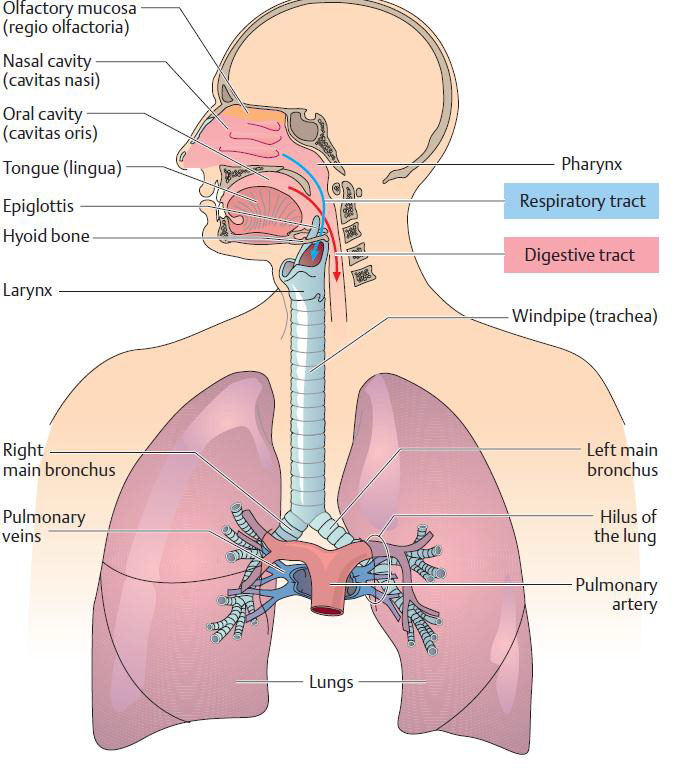
Organs of the Respiratory System
The respiratory system is essential for life. The goals of respiration are to provide oxygen to the tissues and to remove carbon dioxide. The respiratory system consists of mouth or nose, palate, nose, pharynx, larynx, trachea and bronchial which has been discussed on module one session three and the lungs; the principal organ of the respiratory system which will be discussed now. Normal lung function requires a balanced interrelationship between the respiratory (the upper and lower airway), nervous, and cardiovascular systems. The brain receives and sends out stimuli to maintain a normal oxygen and carbon dioxide balance. The medulla and the pons are the major brain centers that affect respiration. The body's respiratory center in the medulla is normally stimulated by an increased concentration of carbon dioxide, and to a lesser extent, by decreased levels of oxygen in arterial blood.
The lungs are found in thoracic cage, this cage is triangular the side walls formed by the ribs and the intercostals muscles its base formed by the diaphragm and the apex of the thoracic cage is in the neck. The pleural cavity is a capillary cavity with little fluid that lies between the visceral pleura that covers the lung and the parietal pleura that lines the inside of the chest wall. The space between the two layers is called the intrapleural space. Because the pressure in the pleural cavity is below atmospheric pressure (intrapleural pressure), while the pressure in the lungs is higher, close to atmospheric pressure, the lung must expand as it follows the inspiratory movements of the thorax and the diaphragm. The fluid in the pleural cavity prevents excessive friction between the two pleural layers.
Mechanisms of Respiration
Mechanisms to achieve the goal of respiration are pulmonary ventilation; the inflow and outflow of air between the atmosphere and the lung alveoli, diffusion of oxygen and carbon dioxide between the alveoli and the blood, transport of oxygen and carbon dioxide in the blood and body fluid to and from the body's tissue cells; and regulation of ventilation and other facets of respiration by the respiratory centre.
The thoracic cavity is made up of 12 pairs of ribs that connect in the posterior thorax to the vertebral bodies of the spinal column.
The lungs lie within the thoracic cavity on either side of the heart, extending from the diaphragm to just above the clavicles or collarbones.
Light, spongy and elastic structures, of the lungs inflate with inspiration and deflate, but do not completely collapse, with expiration.
The right lung is shorter and wider than the left lung. Each lung is divided into lobes - the right lung has three lobes; the left lung has two lobes.
The lung's lobes are further divided into segments. The pleura membranes that cover each lung and line the thoracic cavity.
Mechanics of Pulmonary Ventilation
Normal quiet breathing is accomplished almost entirely by movement of the diaphragm. The diaphragm is principal muscle of respiration which is attached to the inferior margin of the rib cage and to the bodies of the lumbar vertebrae behind.
Inspiration: An active process to move air in to the lungs by enlarging chest cavity and contracting the muscles of inspiration. The enlargement of the chest is in three directions:
- Antero-posterior, i.e. from behind forwards- This is produced by the intercostal muscles drawing the ribs and the sternum forwards.
- Laterally, or from side to side- This is produced by the intercostal muscles drawing the lower ribs upwards and outwards.
- Vertically, or from above downwards- This is produced by the contraction of the diaphragm which pulls the lower surfaces of the lungs downward. The diaphragm accounts for 75% of the tidal volume. The distance the diaphragm moves varies from 1.5 cm to 7 cm during deep inspiration.
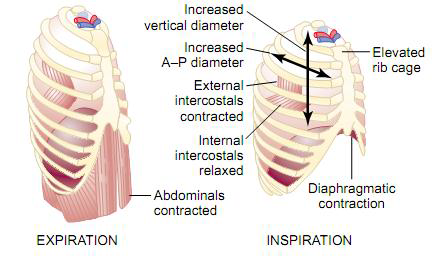
The lungs can be expanded and contracted in two ways: by downward and upward movement of the diaphragm to lengthen or shorten the chest cavity, and by elevation and depression of the ribs to increase and decrease the anteroposterior diameter of the chest cavity
When the chest cavity enlarges, the pressure in the intrapleural space becomes more negative. This expands the lungs and the gases are drawn into the lungs from the atmosphere. For air to enter the lungs at inspiration the pressure gradient must be great enough to overcome the elastic resistance to expansion of the lung and chest wall (total compliance).
The most important muscles that raise the rib cage are the external intercostals, but others that help are the sternocleidomastoid muscles, which lift upward on the sternum; anterior serrati, which lift many of the ribs; and scaleni, which lift the first two ribs.
Expiration is the movement of air out of the lungs to the atmosphere is a passive process. It is not produced by the active contraction of any muscles but by the relaxation of the muscles that were contracting during inspiration. The diaphragm simply relaxes, and the elastic recoil of the lungs, chest wall, and abdominal structures compresses the lungs and expels the air. During heavy breathing, however, the elastic forces are not powerful enough to cause the necessary rapid expiration, so that extra force is achieved mainly by contraction of the abdominal muscles (mainly the abdominal recti), which pushes the abdominal contents upward against the bottom of the diaphragm, thereby compressing the lungs.
Exchange of Oxygen and carbon dioxide between the lungs and the atmosphere: The amount of oxygen in inspired atmospheric air is 21%. The pressure or tension of this oxygen is 158 mmHg (atmospheric total air pressure is 760 mmHg). The inspired air is drawn into the alveoli where it mixes with the air left from the previous respiration. Therefore, the oxygen is diluted, the CO2 raised and water vapor is added. The pressure of O2 in the alveolar air becomes 103 mmHg.
Exchange Between the Blood and the LungsThe venous blood arrives in the lung (from the tissues) with an O2 pressure of 40 mmHg. Because of the difference in pressure (103 - 40 mmHg), O2 passes from the alveoli into the blood stream. This transfer occurs by the process of diffusion. The O2 in solution determines the oxygen tension. It moves from the alveoli where the tension is high to the capillary blood where the tension is low. The capillary blood leaves the lungs after picking up O2 and giving up CO2. It is high in O2 (both dissolved O2 and O2 in combination with hemoglobin). The arterial blood leaves with an oxygen tension of 100 mmHg.
Exchange of Carbon DioxideIn addition to the exchange of oxygen, an exchange of CO2 takes place. The venous blood arriving in the lung is rich in CO2. The pressure of CO2 in the venous blood is 46 mmHg. The alveolar pressure is 40 mmHg. The CO2 diffuses from the venous blood to the alveoli. The arterial blood leaves the lung with an oxygen tension of 100 mmHg and a CO2 tension of 40 mmHg.
Diffusion of gases through the respiratory unit and respiratory membrane:
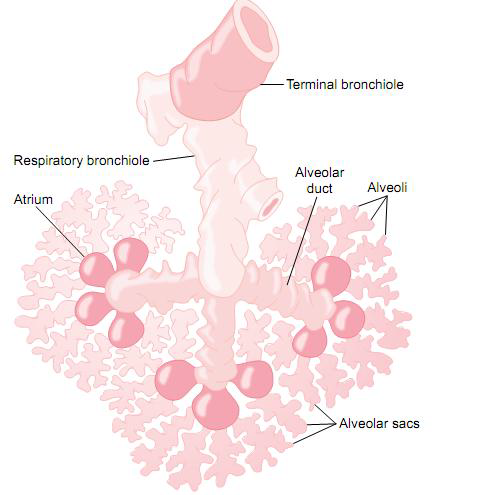
Diffusion: Is the passage of fluid or gas from an area of high pressure across a membrane.
The gases in the alveoli pass into the blood in the capillaries by the process of diffusion.
The respiratory unit is composed of a respiratory bronchiole, alveolar ducts, atria, and alveoli.
There are about 300 million alveoli in the two lungs, and each alveolus has an average diameter of about 0.2 millimeter.
The alveolar lining may be thickened by disease of the lung. The interstitial fluid may be increased in heart disease.
The alveolar walls are extremely thin, and between the alveoli is an almost solid network of interconnecting capillaries. Because of the extensiveness of the capillary plexus, the flow of blood in the alveolar wall has been described as a "sheet" of flowing blood. Thus, it is obvious that the alveolar gases are in very close proximity to the blood of the pulmonary capillaries and the pulmonary blood occurs through the membranes of all the terminal portions of the lungs, not merely in the alveoli themselves. All these membranes are collectively known as the respiratory membrane, also called the pulmonary membrane. If any of these layers is thickened then diffusion is impeded.
Carriage of Oxygen in the BloodOxygen is carried in combination with the hemoglobin in the red blood cells (1 gm of hemoglobin can carry 1.34 ml of O2) and carried in solution (0.3 ml of oxygen per 100ml of blood). When the Hgb combines with O2 it is termed oxyhemoglobin (oxyHb). When it gives up the O2 in the tissues it is termed reduced hemoglobin.
The Passage of Oxygen From the Blood to the TissuesIn the tissues the capillary blood is exposed to a low O2 tension. The oxygen diffuses out of the blood into the tissues. Initially the dissolved O2 in the plasma diffuses out first. When this happens the O2 in combination with the hemoglobin is no longer in equilibrium with the dissolved O2. The O2 passes from the red blood cells (hemoglobin) into the plasma and thence into the tissues. The O2 is thus unloaded into the tissues. There is a relationship between the O2 tension in the plasma and the O2 in combination with the hemoglobin. If the O2 tension is low the O2 content of the hemoglobin will be low. If the O2 tension is high the O2 content of the hemoglobin will be high.
The Respiratory CentreThe respiratory center is composed of several groups of neurons located bilaterally in the medulla oblongata and pons of the brain stem. It is divided into three major collections of neurons: a dorsal respiratory group, located in the dorsal portion of the medulla, which mainly causes inspiration; a ventral respiratory group, located in the ventro lateral part of the medulla, which mainly causes expiration; and the pneumotaxic center, located dorsally in the superior portion of the pons, which mainly controls rate and depth of breathing. The dorsal respiratory group of neurons plays the most fundamental role in the control of respiration.
The Respiratory Ccentre Are Affected By
- Oxygen (O2) lack: Lack of oxygen stimulates the respiratory centre reflex via the chemo-receptors, however oxygen lack directly depresses the respiratory centre. The overall action of oxygen lack on the respiratory centre is stimulation. Respiration is increased and the oxygen lack is minimized.
- Carbon dioxide (CO2) excess or lack: An excess of CO2 stimulates the respiratory centre directly. The respiratory centre is most sensitive to a rise in CO2. The respiratory centre is stimulated not only directly but also through the chemoreceptors. A fall in CO2 can depress the respiratory centre. This is sometimes seen following a general anaesthetic in which the patient has been over ventilated. The respiratory centre is depressed and breathing is slow to return.
- Changes in the acid base balance of the blood: If the acid content of the blood is increased, then the respiratory centre is stimulated.
- Reflex control: e.g., The chemoreceptors (the carotid bodies found at the bifurcation of the common carotid artery and the aortic bodies near the aortic arch) are a special group of cells in the neck. Oxygen lack, carboondioxide excess and increase acidity of blood stimulate the chemoreceptors and cause impulses to travel up these nerves to the respiratory centre.
Lung Volumes
- The tidal volume is the volume of gas passing into or out of the lungs per breath (5-7ml/kg or approximately 500 ml in the average adult).
- Minute volume is the volume of gas passing in or out of the lungs per minute. It is equal to the tidal volume multiplied by the number of breaths per minute.
- Minute volume = Tidal volume x Respiratory rate = 500 ml x 10 rate = 5 liters (in the average adult)
- Dead space is the part of the tidal volume that does not take part in ventilation. It could be considered wasted ventilation in that it serves no useful purpose where gaseous exchange is concerned. There are three types of dead spaces under anesthesia:
- Anatomical dead space: This is the volume of gas that fills the respiratory passages but which is not involved in gas exchange. It extends from the nostrils and mouth down to, but not including, the alveoli. In the average adult this is about 150 ml (2ml/kg body weight). The anatomical dead space is reduced by tracheotomy and end tracheal intubation.
- Physiological dead space: This includes all the air (that for various reasons) does not take part in gas exchange. It includes the anatomical dead space plus air in any of the alveoli into which the blood does not flow and any air in over distended alveoli where gaseous exchange is impaired. Physiological dead space is increased in lung disease.
- Anesthetic dead space: The anesthetic dead space is the volume between the patient and the inflow of fresh gases into the "T piece". If a face mask is used, the dead space is increased considerably because part of the patient's tidal volume occupies the space under the mask and is hence wasted. The use of an endotracheal tube or a tracheotomy tube reduces the dead space.
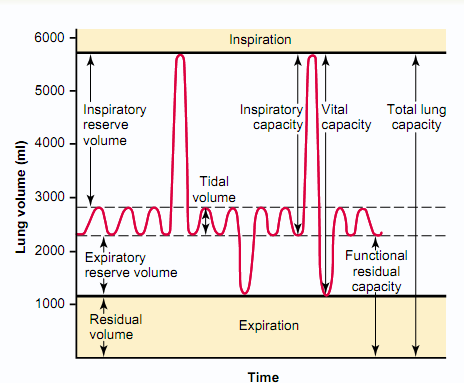
In summery lung capacities are calculated by the following ways
- VC = IRV + VT + ERV
- VC = IC + ERV
- TLC = VC + RV
- TLC = IC + FRC
- FRC = ERV + RV
Alveolar ventilation is that part of the tidal volume that actually takes part in gaseous exchange.
Tidal volume = dead space + alveolar ventilation 500 ml= 150 ml + 350 ml (in 75kg adult).
- Expiratory reserve volume (ERV) is the amount of air that can be forcefully expired at the end of a normal expiration.
- The inspiratory reserve volume is the extra volume of air that can be inspired over and above the normal tidal volume when the person inspires with full force; it is usually equal to about 3000 milliliters.
- Residual volume (RV) is the amount of air remaining in the lungs at the end of a maximum forced expiration.
- Functional residual capacity (FRC) is the volume of air in the lungs at the end of a normal expiration and is the sum of the ERV and the RV.It is important to the anesthetist because it contains a reservoir of oxygen (e.g. after pre-oxygenation and full nitrogen wash-out) which can maintain blood levels of oxygen during apnea. It is decreased by up to 25% in the supine position and also reduced in obesity, pregnancy and under anesthesia.
- The inspiratory capacity equals the tidal volume plus the inspiratory reserve volume. This is the amount of air (about 3500 milliliters) a person can breathe in, beginning at the normal expiratory level and distending the lungs to the maximum amount.
- Vital capacity is the greatest amount of air that can be expired after a person has breathed in as much as possible.
- The total lung capacity is the maximum volume to which the lungs can be expanded with the greatest possible effort (about 5800 milliliters); it is equal to the vital capacity plus the residual volume.
Compliance and Air Way Resistance
Compliance is a measure of distensibility. Lung compliance is defined as the change in volume per unit change in pressure. Airway resistance denotes the measure of obstruction to the flow of gas in the air passages. Flow of gas in a tube depends on a number of factors. Anything that reduces the size of the air passage will interfere with flow and therefore increase the airway resistance. Most of the resistance to air flow is in bronchi greater than 2 mm in diameter. Airway resistance is increased in asthma, emphysema, pulmonary congestion etc. In these conditions the work of breathing is increased.
Common Problems of Oxygenation and Ventilation
Hypoxia Means a Lack of O2 in the Body (Tissues). Hypoxemia is a lack of O2 in the blood. This may reveal itself as blueness of the tissues of the lips, tongue and mucous membranes of the mouth. Hypoxia must be diagnosed quickly and treated aggressively otherwise permanent neurological damage and cardiac arrest may quickly follow. Treatment of hypoxia and hypercarbia is removal of the cause and administration of oxygen.
Types of Hypoxia
- Hypoxic hypoxia: This occurs if the O2 pressure in the blood is reduced for any reason. There is less O2 carried in the blood, both in solution in the plasma and also in combination with the Hgb. The quantity of Hgb may normal. This may occur under anaesthesia when the flow rate of gases used is incorrect, the cylinder is empty and escapes attention or the oesophagus is intubated and not immediately remedied (all inexcusable). It may also occur at a high altitude where inspired O2 is at a reduced pressure.
- Anemic hypoxia: Here there is a reduction in the amount of circulating Hb. If the Hb is reduced then the oxygen carried in the blood is reduced.
- Stagnant hypoxia: This occurs when the circulation is inadequate for any reason. The blood spends a longer time in the tissues and therefore loses more O2 and the venous blood returning to the lungs also has less O2. This is met with in 'shock' where the blood pressure is very low and the circulation sluggish. It also happens in heart failure.
- Histotoxic hypoxia: This occurs when the tissues are poisoned with drugs or chemicals, e.g. in cyanide poisoning. It is also seen if the tissues are edematous. In these situations the tissues cannot accept or use the O2 brought to them by the blood.
- Diffusion hypoxia: This occurs at the end of an anaesthetic where N2O/O2 is used. The nitrous oxide passes out of the blood stream and into the alveoli faster than the nitrogen in air passes in and this may dilute the concentration of inspired O2. If the patient is breathing atmospheric air then this falls to below 20%. This is overcome by giving the patient 100% O2 at the end of the anesthetic.
Hypercapnia
Hypercapnia (PaCo2 > 45mm Hg) occurs during the courses of anesthesia when there is imbalance between production of carbon dioxide and its elimination by alveolar ventilation. In most patients, the usual clinical signs of hypercapnia are not seen during anesthesia because the normal physiologic responses to hypercapnia are obtunded. Hypertension, tachycardia, and the appearance of dysrhythmia can be associated with hypercapnia
Causes of CO2 Excess (Hypercapnia) in Aanaesthetic Practice
- Respiratory obstruction causing inadequate ventilation.
- Inadequate ventilation, due to depression of the respiratory centre or the action of muscle relaxants.
- Faulty CO2 absorption in circle absorbers.
- Accidental administration of CO2.