Anesthetic Breathing System
Anesthetic Breathing System
Function and Classification of Anesthetic Breathing System
The function of anesthetic breathing systems is to deliver oxygen and anesthetic gases to the patient and to eliminate carbon dioxide. Conceptually, the anesthetic breathing system is a tubular extension of the patient’s upper airway. It allows the continuous flow from the anesthesia machine to be converted into an intermittent flow; allows spontaneous, controlled, or assisted respiration; and provides for other functions such as gas sampling and airway pressure, flow, and volume monitoring
Anesthetic breathing systems can add considerable resistance to inhalation. The components of the breathing system, particularly the tracheal tube connector, should have the largest possible lumen to minimize this resistance to breathing. Substituting controlled ventilation of the patient’s lungs for spontaneous breathing can offset the increased resistance to inhalation imparted by anesthetic breathing systems.
Anesthetic breathing systems are classified as open, semiopen, semiclosed, and closed (Table 3.1) according to the presence or absence of:
- Gas reservoir bag in the circuit
- Rebreathing of exhaled gases
- Means to chemically neutralize exhaled carbon dioxide
- Unidirectional valves.
- Fresh gas inflow rate
Table 3.1 Anesthetic Breathing System
| System | Unidirectional valve | Fresh gas inflow rate | Example |
|---|---|---|---|
| Open | No | Unknown | Insuflation Open drop |
| Semiopen | One | high | Non rebreathing circuit e.g., Ayres T piece |
| Semiclosed | Three | Moderate | Circle |
| Closed | Three | Law | Circle |
| High, greater than 6 L/min; moderate, 3 to 6 L/min; low, 0.3 to 0.5 L/min. No rebreathing of exhaled gases only when fresh gas inflow is adequate. |
|||
Table 3.2 Anesthetic Breathing System
| System | Breathing bag | Rebreathing | Co2 absorber |
|---|---|---|---|
| Open | No | No | No |
| Semiopen | Yes | Partial | No |
| Semiclosed | Yes | Partial | Yes |
| Closed | Yes | Total | Yes |
| High, greater than 6 L/min; moderate, 3 to 6 L/min; low, 0.3 to 0.5 L/min. No rebreathing of exhaled gases only when fresh gas inflow is adequate. |
|||
Table 3.3 Mapleson Breathing Systems
| Type of Circuit | FGF for spontaneous ventilation | FGF for spontaneously breathing 70kg patient |
|---|---|---|
| A | > alveolar minute ventilation (85mL/kg/min) | 6 L/min |
| B | 1.5 x minute ventilation (150mL/kg/min) | 10 L/min |
| C | ||
| D | 2 x minute ventilation (200mL/kg/min) | 14 L/min |
| E | 2-3 x minute ventilation | Always > 3 L |
| F |
Table 3.4 Mapleson Breathing Systems
| Type of Circuit | FGF for controlled ventilation | FGF for 70 kg patient with controlled ventilation |
|---|---|---|
| A | 2.5 x minute ventilation (250mL/kg/min) | 17 L/min |
| B | 1.5 x minute ventilation (150mL/kg/min) | 10 L/min |
| C | ||
| D | >alveolar minute ventilation (85mL/kg/min) | 6 L/min |
| E | - | - |
| F | 1000mL +100 mL/kg | Not available |
Sample of Open System- Insufflation
Insufflation: The term insufflation usually denotes the blowing of anesthetic gases across a patient's face. Although insufflations is categorized as a breathing system, it is perhaps better considered a technique that avoids direct connection between a breathing circuit and a patient's airway. Because children often resist the placement of a face mask or an intravenous line, insufflation is particularly valuable during pediatric inductions with inhalation anesthetics. Ventilation cannot be controlled with this technique, however, and the inspired gas contains unpredictable amounts of entrained atmospheric air. Figure 3.1

Sample of Semiopen System - The T-Piece and Bain Circuit System (Table 3.2)
The Mapleson F (Jackson-Rees) system (Figure 3.2) is a T-piece arrangement with a reservoir bag and an adjustable pressure-limiting overflow valve on the distal end of the gas reservoir bag. The venting piece is usually a valve with an adjustable orifice that is connected to waste gas scavenging system. During inspiration the patient breathes fresh gas from the machine and gas stored in the expiratory limb. During exhalation, a mixture of exhaled and fresh gas collects in the bag. On the next inspiration the patient inhales fresh gas from the machine and that stored in the expiratory limb. Fresh gas flow equal to two to three times the patient's minute ventilation is recommended to prevent rebreathing of exhaled gases.

These are: Popular in pediatric Elimination of carbon dioxide is accomplished by removing all expired gases from the system and venting them to atmosphere. Because relatively high fresh gas flows are needed, all T-piece systems are less desirable for use in adults. They also cause greater loss of moisture from the airway if dry gases are used.
The Bain Vircuit (Figure 3.3): in which the fresh gas supply tube runs coaxially inside the corrugated expiratory tubing. The fresh gas tube enters the circuit near the reservoir bag, but the fresh gas is actually delivered at the patient end of the circuit. The exhaled gases are vented through the overflow valve near the reservoir bag. The Bain circuit may be used for both spontaneous and controlled ventilation. Prevention of rebreathing, inhale previously respired gases from which carbon dioxide may or may not have been removed, during spontaneous ventilation requires a fresh gas flow of 200 to 300 mL/kg/min and a flow of only 70 mL/kg/min during controlled ventilation.
Advantages of the Bain circuit include:
- Warming of the fresh gas inflow by the surrounding exhaled gases in the corrugated expiratory tube.
- Conservation of moisture as a result of partial rebreathing
- Ease of scavenging waste anesthetic gases from the overflow valve. It is lightweight, easily sterilized, reusable, and useful when access to the patient is limited, such as during head and neck surgery.
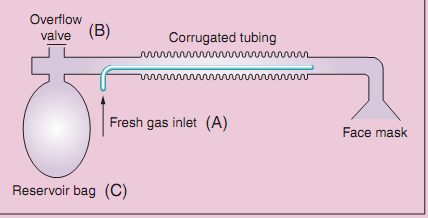
Disadvantages: Hazards of the Bain circuit include unrecognized disconnection or kinking of the inner fresh gas tube. The outer expiratory tube should be transparent to allow inspection of the inner tube.