Treatment of uncomplicated malaria based on RDT confirmation
Scenario 1
If RDT indicates P. falciparum infection then treat the patient with appropriate doses of Coartem (one of the artemisinin-based combination drugs), or artemisinin combination therapy with chemical ingredients of artemether-lumefantrine. Before you give the patient Coartem, make sure that the patient is able to swallow the medication, and is not vomiting. (See the treatment doses of Coartem in Table 8.1). Coartem tablets are given according to the body weight or age of the patient, in six doses to be taken over three days. Give the first dose to the patient in front of you. Advise your patient to take fatty foods if available. If fatty food is not available, advise the patient to take any foods or fluids after swallowing Coartem. Explain that a fatty meal or milk improves absorption of Coartem, hence the patient can recover faster.
One tablet of Coartem contains 120 mg artemether, plus 20 mg lumefantrine, in a fixed dose.
Table 8.1 Coartem treatment doses and schedules by body weight and age.
| Weight (kg) | Age | Day 1 | Day 2 | Day 3 | |||
|---|---|---|---|---|---|---|---|
| Morning | Evening | Morning | Evening | Morning | Evening | ||
| 5-14 | 4 months-2 years | 1 tablet | 1 tablet | 1 tablet | 1 tablet | 1 tablet | 1 tablet |
| 15-24 | 3-7 years | 2 tablets | 2 tablets | 2 tablets | 2 tablets | 2 tablets | 2 tablets |
| 25-34 | 8-10 years | 3 tablets | 3 tablets | 3 tablets | 3 tablets | 3 tablets | 3 tablets |
| 35+ | 10 + years | 4 tablets | 4 tablets | 4 tablets | 4 tablets | 4 tablets | 4 tablets |
Scenario 2
If the RDT indicates mixed infection of P. falciparum and P. vivax, then treat the patient with appropriate doses of Coartem, as in Table 8.1.
Scenario 3
Chloroquine tablets are 150 mg base, and the syrup is 50 mg base per 5 ml dose.
If the RDT reveals P. vivax only, then treat the patient with Chloroquine (see the treatment doses in Table 8.2). Chloroquine is prepared in tablet or in syrup form. Chloroquine dose is 10 mg/kg of the patient's body weight, taken orally immediately (day 1), followed by 10 mg/kg at 24 hours (day 2), and 5mg/kg at 48 hours (day 3).
How many tablets of Chloroquine to take home do you give to a woman aged 36 years who is diagnosed with P.vivax malaria? Note that you give her the first dose, i.e. 4 tablets, while she is in front of you.
Table 8.2 Chloroquine treatment doses (tablets or syrup) and schedules by body weight and age.
| Weight (kg) | Age | Day 1 | Day 2 | Day 3 |
|---|---|---|---|---|
| 5-6 |
less than 4 months |
1/2 tablet OR 5 ml syrup |
1/4 tablet OR 5 ml syrup |
1/4 tablet OR 2.5 ml syrup |
| 7-10 |
4-11 months |
1/2 tablet OR 7.5 ml syrup |
1/2 tablet OR 7.5 ml syrup |
1/2 tablet OR 5 ml syrup |
| 11-14 |
1-2 years |
1 tablet OR 12.5 ml syrup |
1 tablet OR 12.5 ml syrup |
1/2 tablet OR 7.5 ml syrup |
| 15-18 |
3-4 years |
1 tablet OR 15 ml syrup |
1 tablet OR 15 ml syrup |
1 tablet OR 15 ml syrup |
| 19-24 |
5-7 years |
11/2 tablets OR 20 ml syrup |
11/2 tablets OR 20 ml syrup |
1 tablet OR 15 ml syrup |
| 25-35 |
8-11 years |
2 tablets |
2 tablets |
1 tablet |
| 36-50 |
12-14 years |
3 tablets |
3 tablets |
2 tablets |
| 51+ |
15 + years |
4 tablets |
4 tablets |
2 tablets |
Scenario 4
If the RDT is positive for P. falciparum in:
- women who are less than 3 months pregnant,
- children whose weight is less than 5 kg or whose age is less than 4 months,
give quinine oral treatment. (See the treatment doses of quinine tablets in Table 8.3 below).
Quinine tablets may contain 200 mg or 300 mg. Check carefully when you calculate the dose.
Table 8.3 Quinine treatment doses by body weight and age.
| Weight (kg) | Age | Dosage to be given daily | |
|---|---|---|---|
| 200 mg tablets | 300 mg tablets | ||
| 4-6 | 2-4 months | 1/4 | - |
| 6-10 | 4-12 months | ⅓ | 1/4 |
| 10-12 | 1-2 years | 1/2 | ⅓ |
| 12-14 | 2-3 years | 3/4 | 1/2 |
| 14-19 | 3-5 years | 3/4 | 1/2 |
| 20-24 | 5-7 years | 1 | 3/4 |
| 25-35 | 8-10 years | 11/2 | 1 |
| 36-50 | 11-13 years | 2 | 11/2 |
| 50+ | 14 years and above | 3 | 2 |
For all of Scenarios 1 to 4, if the patient vomits within 30 minutes after swallowing the drug, the medicine will not work. So give the patient the same dose again from your own stock (not from the tablets you give to the patient or the mother/caregiver to take home) and let the patient swallow it.
If a child vomits within 30 minutes of taking drugs at home, advise the patient/caregiver to take another dose, and to come back to the Health Post to collect another replacement dose from you so that the patient still takes the complete course of treatment.
To ensure appropriate intake of prescribed drugs, patients/ caregivers should be well informed on the treatment schedule to ensure intake of the complete dose.
Advise the patient/caregiver to come back if the patient does not show any improvement after three days of treatment with anti-malaria drugs, or if the signs and symptoms get worse at any time.
Whenever you encounter a suspected malaria case, use the guide in your textbooks on the procedures and steps that you need to follow to identify uncomplicated and severe malaria cases using RDTs, and manage them appropriately.
If the RDT result of Bekele, who is a 7-year-old child, shows P. falciparum infection, what anti-malaria drug would you give him? How many tablets will be a complete course of treatment? If Bekele vomited 25 minutes after swallowing the first dose you gave him, what should you do next?
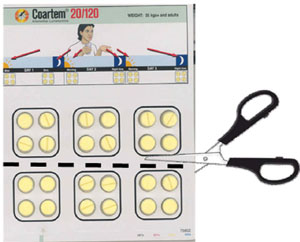
The total number of tablets you give a 7-year-old child is 12 (go back to see the doses in Table 8.1 above). The Coartem strip that contains 12 tablets is shown in Figure 8.2. Bekele should be given 2 tablets in the morning and 2 tablets in the evening for 3 days.
To replace the vomited dose, which is 2 tablets, give the child another 2 tablets to swallow again from your own stock -- not from the tablets you gave to the mother/caregiver. The mother/caregiver must have 10 tablets to take home to continue the treatment.
Note that if the strip in Figure 8.2 (which is appropriate for Bekele) is not available, you can still cut out 12 tablets from the strip of adult doses as shown in Figure 8.3. While cutting the strips be careful not to cut the plastic or the blisters that contain individual tablets.
Coartem shelf life and contraindications
Coartem has a short shelf life of two years only. So use those packages which are closer to the expiry date first. Do not expose Coartem to moisture and high temperature. Store it at temperatures of below 30oC in dry and cool places.
Coartem absorbs moisture from the surrounding environment very fast. To protect the drug from absorbing the moisture it is covered by plastic blisters. Therefore, do not remove the tablet from the blister if it is not going to be used immediately.
Coartem is contraindicated (not given) for some people. Box 8.2 gives you specific warnings on the groups who should not get Coartem.
Box 8.2 Contraindications of Coartem
Previously, Coartem was contraindicated for breastfeeding mothers of infants less than 5 kg or under 4 months old. WHO Malaria Treatment Guidelines, 2010, now state that Coartem should be given to these patients.
Do not give Coartem for the following groups of people:
- For use as prophylaxis, that is for a healthy person who wants to swallow the drug in order to protect himself or herself from getting malaria
- Pregnant women in the first trimester (three months of pregnancy) and infants less than 5 kg or less than 4 months old
- Persons with a previous history of reaction after using the drug.