How to use an RDT to get a malaria test result
Here is the checklist that you must follow when you are using an RDT for malaria diagnosis.
(i) Check the expiry date on the package. Do not use RDTs that have expired.
(ii) Put on gloves before beginning (Figure 7.3). Use a new pair of gloves for each patient. Do not re-use gloves.

Figures 7.3 to 7.10 are from WHO, 2006, How to Use a Malaria Rapid Diagnostic Test (RDT): A Guide for Training CHWs and Other Health Workers.
(iii) Open the RDT package and remove the contents. The blood-transfer device — it could be a capillary tube, straw, loop, pipette or other device — is used to collect blood and transfer it to the test cassette. (Once the packet is opened, the 'desiccant' sachet which absorbs moisture from the atmosphere in the package should be discarded.) The test cassette (shown later, in Figure 7.8) is used to conduct the test. The square hole labeled 'A' is where you add the blood. The round hole labeled 'B' is where you add the buffer.
(iv) Write the patient's name on the cassette (Figure 7.4).

(v) Open the alcohol swab and clean the patient's third or fourth finger with alcohol (Figure 7.5). This is to prevent infection. Other fingers may be used if necessary. Ask the patient: 'Are you right-handed or left-handed?' If the patient is right-handed, choose a finger on their left hand. If the patient is left-handed, choose a finger on their right hand.

(vi) After cleaning the finger with the alcohol swab, the finger must be allowed to air dry. After using the alcohol swab, place it on its wrapper and set it aside on the table. You will use it again to stop the bleeding after you collect the patient's blood.
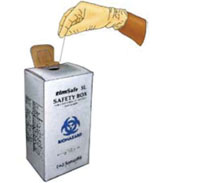
(vii) Once the patient's finger is dry, open the lancet. Prick the patient's finger, preferably towards the side of the pulp (ball) of the finger. Discard the lancet in a sharps-only container immediately after using it (Figure 7.6).
Never put the lancet down before discarding it. Never discard the lancet in a non-sharps container. Never use a lancet on more than one person.
(viii) Turn the 'patient's' arm so their palm is facing downward. Squeeze the pricked finger and allow a drop to well up below the finger tip as in Figure 7.7. Use the loop or capillary tube or straw or the pipette to collect the drop from underneath. Once you have collected a sufficient amount of blood, you may hand the alcohol swab back to the patient and show him or her how to use it to stop the bleeding.

(ix) Use the device (capillary tube, straw, loop, pipette or other) to add the drop of blood to the sample window (square hole labeled with the letter A, see Figure 7.8). The blood needs to reach and be absorbed by the pad at the base of the square hole. If the blood is mostly deposited on the plastic edges of the well, but does not reach the pad, the test will not work correctly. Deposit the blood in the correct place using the capillary tube, straw, loop, pipette or other. Adding too much or too little blood can cause the test to give an invalid result or be difficult to read.

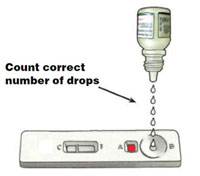
(x) Add the buffer solution to the round hole labeled B. Hold the bottle vertically when adding the buffer solution, as in Figure 7.9. This ensures the correct drop size.
(xi) Wait for the correct duration of time (15 or 20 minutes) after adding buffer before reading the test results.
(xii) Discard the blood-collection device (e.g. capillary tube) safely after use.
(xiii) Remove and discard your gloves at this time. To avoid possible contamination, the used gloves should be discarded in the non-sharps container before you do anything else.