Care for young women during pregnancy
What are the risks for a young woman's health if she becomes pregnant?
If a young woman becomes pregnant, she could face many health risks including malnutrition and hypertension (raised blood pressure). Then there is the danger that she has a premature baby, a prolonged and obstructed labour leading to complications like fistula and/or that her baby is stillborn.
What is the reason for these problems?
As you learned in Study Session 3 of this Module, young women may not have completed their growth so the pelvis (the bone surrounding the birth canal) is often still growing and immature which makes giving birth difficult. They may not have enough food and when the baby starts to grow, mother and baby will be in competition for what little food there is, so both will be malnourished.
In Study Session 13 (Providing Focused Antenatal Care) of the Antenatal Care Module you learned that pregnancy is particularly risky for girls who are less than 16 years old. For them, in particular, childbirth may be difficult if the pelvis is still growing because it will be too small for the baby to pass through it easily (remember this is called obstructed labour).
In areas where health facilitates are inaccessible, the young woman may face an unassisted and lengthy labour which can lead to tearing or rupture of the uterus. She may die of blood loss (haemorrhage).
During a lengthy labour, the baby's head can stretch or tear the vagina causing a hole between the vagina and the bladder or between the vagina and the rectum. This hole is called a fistula.
If the baby can't pass out of the body a cut in the woman's abdomen will be made so that the baby can be lifted out of the uterus. The doctors call this operation a Caesarean section.
To avoid complications in pregnancy young women need to go for antenatal care as soon as they know they are pregnant. If you are aware of any pregnant young women in your area, you should encourage them to follow a schedule of regular antenatal care visits. If they are under 16 years old you should refer them to a higher facility for antenatal care.
What is the basic number of visits provided with focused antenatal care (FANC)?
A woman should commonly have four FANC visits and the first visit should ideally be during the first trimester (the first three months of the pregnancy) but certainly by 16 weeks. The second visit should be made during the fourth to sixth months of pregnancy. Third and fourth visits should be in the eighth and ninth months respectively.

Activity 11.1 The FANC plan
Do you remember what you should do for the pregnant women during each visit?
In Table 11.1 write down the specific activities you should carry out at each visit.
Here are some principles that will help you complete the table.
- Every pregnancy is a risk.
- Antenatal care (ANC) should be used as a main gate for health promotion and disease prevention.
- ANC must be used as an opportunity to detect and treat existing problems.
- ANC must be used to prepare pregnant women, their partners and families to plan the birth preparedness and complication readiness plan.
You should also remember that the ANC service should be individualised: every woman should be counselled and treated according to her specific needs.
Table 11.1 Activities carried out during each FANC visit.
| First visit (when pregnancy is confirmed) | Second visit (4–6 months) | Third visit (8 months) | Fourth visit (9 months) |
|---|---|---|---|
When you have completed Table 11.1 refer to Table 11.2 at the end of this study session to see the things that you need to do at each visit.
When you are planning the care for a pregnant young woman, you should follow the same guidelines as for any other pregnant woman (i.e. use the chart that is shown in Table 11.2). However, you should give much more attention to your counselling role as a young woman has more specialised needs than an adult.
On what specific issues should you counsel a pregnant woman? (You have learned this in the Antenatal Care Module.)
You should educate and counsel pregnant women on the following topics:
- Protecting themselves from malaria by sleeping under an insecticide-treated bed net (ITN)
- Eating a balanced diet with nutritious food (refer to the Nutrition Module)
- Prevention of mother to child transmission of HIV (PMTCT)
- Personal hygiene
- Taking adequate rest
- Breastfeeding
- Harmful traditional practices (HTPs) that relate to pregnancy, birth and care of the baby
- Warning signs and danger symptoms during pregnancy.
All these topics are discussed in the Antenatal Care Module.
Stop reading and think about whether there are specific HTPs practised in your community that could damage the health of the pregnant mother or the baby.
If the young woman is in a polygamous marriage she may not be given enough to eat; malnutrition is damaging to her and her baby. The baby will be at risk if colostrum (the thin, watery fluid produced by her breasts during the first three days of her new baby's life) is thrown away and the baby is fed other liquids and honey. You may have thought of other HTPs.
You need to counsel young woman on danger symptoms without frightening them. They should know the symptoms for which they should seek immediate help. Give reassurance and tell them about only the danger symptoms that it is appropriate to know about for the stage of their pregnancy.
What are the danger symptoms they should seek help for in the period up to 20 weeks?
Symptoms that are dangerous and should be taken seriously and responded to include vaginal bleeding, persistent vomiting, fever, no change in abdominal growth.
What are the additional danger symptoms they should seek help for in the period after 20 weeks?
Convulsions, leakage of amniotic fluid, headache, burning epigastric pain(see Figure 11.1).
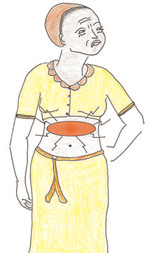
Every woman should deliver with the assistance of a skilled attendant. Although you can provide good help during childbirth you need to make every effort to enable young women to deliver in a higher health facility. Pregnant adolescents who are under 16 years of age are at particularly high risk and should always be referred for delivery to the next higher level health facility (Figure 11.2).

During antenatal visits you should help young women to develop a birth plan that focuses on:
- What to do if any danger symptoms occur
- How they will get to the healthcare facility
- When to check in with the health facility if they suspect that labour is beginning
- Who will provide physical and emotional support during labour.
You also need to prepare the young woman and her supporter(s) by giving them all the necessary information and techniques to make labour more comfortable.
