Neonatal resuscitation
Asphyxia (shortage of oxygen) in the uterus is due to an inadequate supply of oxygen from the mother's blood or a problem in the placenta. This may result in
- Asphyxia at birth (mild, moderate or severe).
- Learning difficulties or cognitive impairment, which become apparent during childhood development; they are due to brain cells being destroyed by lack of oxygen during labour and delivery.
- Death of the newborn.
Most babies breath spontaneously after birth but some babies may not. If a spontaneously breathing baby sustained breathing immediately after birth it indicates that:
- The baby was not asphyxiated in the uterus.
- The newborn's respiratory system is functioning well.
- The newborn's cardiovascular system is working well.
Some babies who have no adequate oxygen due to bleeding from birth trauma or those remained cyanotic (bluish discoloration of the body) may require resuscitation despite their breathing established.
Degrees of Asphyxia
Moderate to severely asphyxiated babies usually need intensive resuscitation, so the next thing we are going to see is how to grade asphyxia in a newborn. Within no more than 5 seconds after the birth, you should make a very rapid assessment to find out whether the baby is alive or dead, and (if it is alive) to assess whether it has any degree of asphyxia.
A severely asphyxiated baby may not breathe at all, there may be no movement of its limbs (arms and legs), and the skin colour may be intensely blue or genuinely white. A baby who is not breathing at all after birth, or, who is breathing less than 30 breaths per minute needs help immediately. If a baby does not breathe soon after birth, it may get brain damage or die.
Most babies who are not breathing can be saved if resuscitation is correctly applied.
Things you should know before you initiate resuscitation:
- Is the fetus alive?: If the fetus does not appear to be alive, listen to the fetal heartbeat on stethoscope, if not heard it means that the fetus died
- The grade of asphyxia: If you can listen to the heartbeat, but you estimate it to be less than 60 beats/minute, apply a heart massage first, then ventilate alternately on and off, till the heartbeat is above 60 beats/minute.
- No meconium intensely stained on the baby: If the baby's skin is stained with meconium or the oral and nasal cavities are filled with meconium stained fluid, you should not resuscitate before suctioning the oral, nasal and pharyngeal areas. Ventilation will aggravate the baby's breathing problem because it will force the meconium-stained fluid deep into the baby's lungs, where it will block the gas exchange.
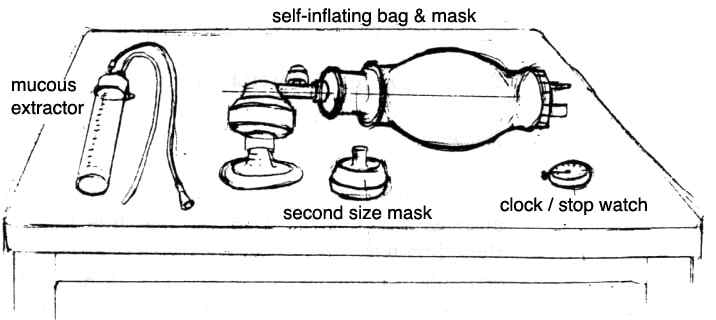
Equipment required to perform neonatal resuscitation (Figure 7.6).
- Two clean linen or cotton cloths: one to dry the newborn and one to wrap him ] afterwards, including the head.
- A plastic bulb syringe to remove the secretions from the mouth and nose, especially when meconium is present.
- An Ambu-bag and mask to give oxygen directly into the baby's lungs.
- A trained person in neonatal resuscitation area.
- A heat source (lamp) to provide some warmth, if possible.
Types of Resuscitation
There are different types of resuscitation procedures that include:
- Suctioning: is the extraction of secretion from the mouth and nose using an instrument called a bulb syringe (Figure 7.7).
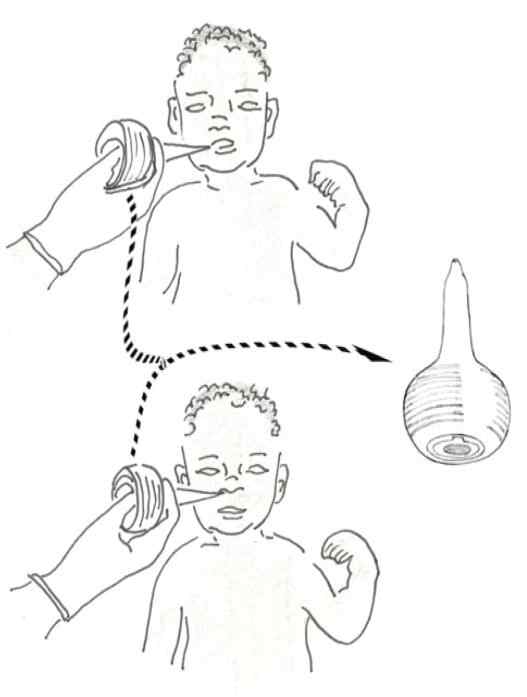

First, you should compress the bulb syringe, then insert it 5 cm into the mouth. Then, you should release the pressure from the bulb syringe and let it suck the mucus and fluids in the mouth. Then, you should remove the bulb syringe and expel the mucus outside.
The same procedure should be applied with the nostrils. However, the bulb syringe can only be inserted 3 cm into the nose.
(Remember: Do not suction deep into the throat as this may cause the heart to slow or breathing to stop)
- Ventilation: initiation of breathing using an instrument called Ambu bag (hand-operated and used to deliver oxygen). The Ambu-bag has a mask piece that needs to be adjusted to the mouth and nose to pump air into the fetal lung (Figure 7.8 below).

- Heart massage: pressing the fetal heart gently with your hand thumbs or with the middle and index finger in a rhythmic way to stimulate the heart beat. Important: NEVER attempt to give a heart massage because you might injure the sternum and ribs.
Neonatal Resuscitation Procedures
- The first five seconds: this indicates what you will do in the first five seconds immediately after birth based on the fetal condition. The following are the summary of fetal, responses to the stimulus and condition with possible degree of asphyxia and management
- If the newborn is crying and moving the limbs; he/she is probably healthy (no asphyxia ) and does not require resuscitation.
- If the newborn has a weak breathing, not moving the limbs, a moderate cyanosis; Then, the baby is probably moderately asphyxiated and requires ventilation by on an off.
- If the newborn is not crying, not breathing, not moving the limbs, floppy, cyanosed or meconium stained, then, the baby is probably severely asphyxiated and requires immediate resuscitation; call for help and estimate the fetal heartbeat (FHB). If the FHB is more than 60 beats/minute, do suction, then ventilation on- off. If the FHB is less than 60 beats/ minute, do heart message, then ventilation on - off.
- Checking the newborn's heart rate: The apical heartbeat (or AHB) is just another name for the heartbeat heard with a stethoscope over the area of the heart on the left side of the chest, so-called apical heartbeat, as it is heard directly over the heart (Figure 7.8). The newborn's heartbeats can be counted with the fetoscope or stethoscope at the apical area or feeling the pulse at the base of the umbilical cord.
- Dry the baby quickly and keep it warm; dry the baby immediately with one towel and cover another dry towel. Make skin contact with the mother and cover the baby with a blanket. Make sure you cover the head to prevent heat loss. Use a heat lamp, if available.
- Clearing the mouth and nose; suction the mouth, then the nose with a bulb syringe, if available or with a dry cloth.
- Apply a gentle tactile stimulation to initiate or enhance breathing; you can stimulate the newborn by gentle rubbing the baby's abdomen up and down, or you may rub the underside of the baby's foot with your fingers.

You should not do:
- Slap the back.
- Squeeze the rib cage.
- Force the baby's thighs into its abdomen.
- Dilate the anal sphincter (the ring of muscle that closes the anus).
- Put hot or cold compresses or baths.
- Shake the umbilical cord.
- If you diagnose asphyxia, start resuscitation immediately.
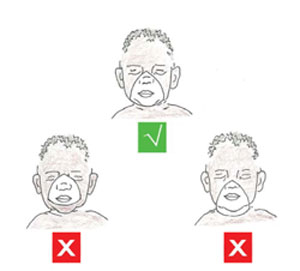
Put the baby in back position with the neck slightly extended. Then open the airway removing mucus and secretions. Initiate ventilation with an Ambu-bag. You should be situated at the head of the baby, and you should look at the fetal chest movement with each ventilation.
Make sure that the mask fit well and covers the mouth, nose and chin and no air escapes between the mask and the face. Do not force the mask to the face because this will cause a downward movement of the chin toward the chest and compress the airway. Check the AHB of the newborn. If the AHB is less than 60 beats/minute; start heart massage with ventilation alternatively (on and off ventilation).
- Ventilate at 40 breaths per minute
Count out loud: "Breathe " two - three" as you ventilate the baby. Two for releasing and three for getting ready for the next breath. This will help you ventilate with an equal rhythm, at a rate that the newborn's lungs are naturally adapted to.When you are doing so, you are ventilating the neonate with a rate of 40 breaths / minute. Apply enough pressure to create a noticeable gentle rise and fall of the baby's chest. The first ventilation requires a higher pressure but note that deep breathing is indicator that you applied much pressure
- Evaluate the baby during ventilation
The signs of good ventilation and improvement in the baby's condition are the following:
- An increased heart rate (>100 beats/minute). This is the best indicator for proper ventilation and improvement in newborn's condition.
- The newborn looks pinkish.
- Moves the limbs.
- Breathes spontaneously or cries as you stop ventilating.

Summary of the Newborn Resuscitation Procedure
| Position |
|
|---|---|
| Clear airway |
|
| Ventilate |
|
| Monitor |
|

How to Ventilate
- Squeeze the Ambu-bag with two fingers or with the whole hand, 2-3 times.
- Observe for rising of the chest.
- If the chest is not rising:
- Reposition the head.
- Check the mask seal.
- Squeeze the bag harder with the whole hand.
- Once you a have a good seal and the chest rising, ventilate at 40 squeezes per minute.