Assessment of a woman in labour
In this section we are going to see how you assess, the component of rapid assessment in women in labour and equipment required to evaluate women in labour.
Conducting a rapid assessment of a woman in labour
As usual, whenever you encounter women in labour you should do a rapid assessment to know the progress of labour and emergency conditions that necessitate urgent referral.
What Is the Equipment You Need to Assess Women in Labour Rapidly?
- ANC card (if she had followed up) if it is first and already in labour record her data on health card.
- B/P apparatus to monitor the blood pressure.
- Fetoscope to measure fetal heart beat.
- Watch to count fetal heart rate and maternal pulse
- Partograph to monitor the progress of labour.
- Sterile glove for vaginal examination.
- Swabs (3-4 swabs soaked with savlon or chlorhexidine 2-4%) to clean the perineum before performing a vaginal examination or you can use soap and boiled water.
![]()
Never use alcohol to clean the perineum. As it cause dryness and irritation of the vaginal mucosa!.
Preventing Mother to Child Transmission (PMTCT)
At this section, we are going to discuss how to provide PMTC service to a labouring mother. This is especially for those mothers who do not know their Human Immune Deficiency Virus (HIV) status, mothers who do not attend ANC follow up, for those who arrive at the time of labour and mothers missed the opportunity of being attended by ANC. The aim is to diagnose any labouring mother for the presence of HIV in their blood and if found positive refer them for further investigation and initiation of Anti Retro Viral Therapy (ART). To provide this service, first, you should offer the mother HIV test and finally counsel the mother based on the result of the test. It is also crucial to keep confidentially (keep the results of the test a secret and do not tell anybody without her consent). You could also refer to module 9, study session 12 for further reading.
Ask About Her Present and Past Pregnancy History
You should ask the mother about her:
- Parity: the number of birth given excluding abortion.
- Gravidity: the number of pregnancy irrespective of its outcome.
- Last normal menstrual period (LNMP): refers to the first day of her last menstrual cycle. If she does not remember to ask her when she felt first fetal movement which is felt around16-18 weeks in multi-gravida and 18-20 weeks in prime-gravida and calculate the expected date of delivery (EDD) if the LMP doesn't pass pagume, add 10 days to the date column and 9 to the month column. If the LMP passes pagume, add 5 days to the date column minus 3 to the month column.
Example: if her LMP was
\( \frac{1/1/2007\\10/9}{11/10/2007} \) \(\frac {4/6/2007\\5/3}{} \)
Her EDD will 9/ 3/2008
You should also ask her about the danger signs, including:
- Vaginal bleeding (heavier than the show).
- Persistent frontal headache.
- Blurring of vision.
- Convulsions.
- Loss of consciousness.
- Epigastric or severe abdominal pain.
- Fever.
- Leakage of amniotic fluid before the onset of abnormal labour and
- Vaginal discharge.
Physical Examination in Labour
Physical examination in labour mainly focuses on abdominal and vaginal examination.
Check the vital signs:
- Check her blood pressure: refer if there is a deviation from the normal range, especially if the diastolic blood pressure (DBP) is > 90 mmhg.
- Count the maternal pulse rate: It should not be greater than110 beats/minute
- Check temperature: average 37ºC; watch out for an increase in body temperature.
Abdominal examination:
The abdominal examination is necessary to determine the position, presentation and lie of the fetus. It is a crucial part of the rapid assessment of women in labour. The following are the steps you should take during the abdominal examination.
- Inspection: this is observing/inspecting the three S (shape, size, skin change and scar) on abdominal examination as you have learned in Module 9.
- Shape: is it large or small for gestational age?. Consider factors that cause a large uterus such as twins, polyhydramnios (amniotic fluid >1500 ml). A small uterus for the gestational age may indicate that the child has not developed well. Both large and small abdomen needs further investigation, and you should refer the mother to the health centre.
- Size: it is important to know the lie (the relation of the fetal long axis to the long axis of the mother) of the fetus. If the shape of the abdomen is ovoid (like an egg) at near to full term or labour, it indicates the baby is presenting with the head. While if it is round like a ball, it may show an abnormal presentation.
- Scar: inspect if the mother had had previous surgery of lower abdomen usually above the pubis that is caesarian section. You should refer those who had previous caesarian section urgently as the chance of giving birth vaginally is very low, and scarring of the uterus puts her at risk of uterine rupture during the current delivery.
- Skin changes -linea nigra- a black line from the above symphysis pubis to the umbilicus. Striae graviderium which is pinkish in primigravida and whitish in multigravida.
- Palpation:
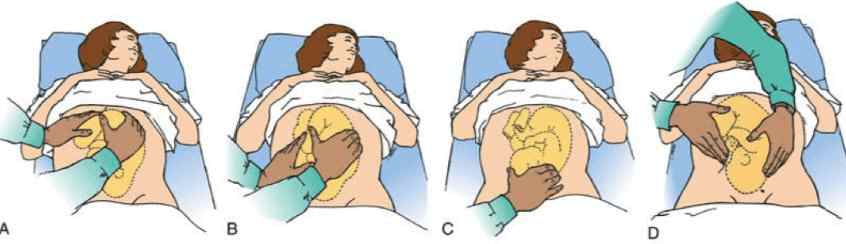
There are four abdominal palpation techniques as you have already learned in Module 9. They are also called the four Leopold Manoeuvres. Look at fig. 2.5 below.- First Leopold manoeuvre - fundal palpation
- This helps to estimate the period of gestation age (GA) & the presenting part that occupies the. The amount of amniotic fluid, maternal size and parity may also affect the estimation.
- Let the mother lie on her back locate the position of the fundus (upper part of the uterus) then measure the height of the fundus using non-elastic tape meter (or your finger if the tape meter is not available) from above the pubic bone to the fundus.
- Each of your fingers is estimated to be 2 cm above the umbilicus and at the level of the umbilicus, it is estimated 20 weeks. If your finger is estimated to be 1cm when the fundus is below the umbilicus.
- Second Leopold manoeuvre- lateral palpation
- It is used to locate the fetal back to determine position. This is important to auscultate fetal heart beat as it is best heard at the fetal back. Place the hands on either side of the abdomen at about umbilical level. Steady the uterus with one hand and the opposite hand palpate the side of the abdomen using a rotary movement. The same movements should be repeated on the other side. This helps you to detect which side of the uterus offers the greater resistance. The back is felt as a curve smooth, resistant mass, and the limbs felt as small irregular parts that slip with the examining finger on the other side
- First Leopold manoeuvre - fundal palpation
- Third Leopold manoeuvre - deep pelvic palpation
- It helps to diagnose the presentation and engagement of the presenting part and also help to determine the attitude of the presentation.
- Ask the woman to bend her knees slightly to relax the abdominal muscles. Turn your body to face the mother's feet. Grasp the uterus below umbilical level between the palms of the hand with fingers, Held close together, pointing downwards and inwards. If you find hard round part, it could be cephalic presentation, and if you feel soft, irregular part, it is breech presentation, which is abnormal you should refer to higher health facility
- Pawlik's grip manoeuvre
- The main aim in this manoeuvre is to judge whether the fetal head descended and engaged but you should be careful not to apply unusual pressure as this can injure fetal head which is not developed well.
- Grasp the lower pole of the uterus between the thumb & fingers of one hand. It should be spread wide enough apart to accommodate the fetal head. The extent of engagement is estimated by how many fingers you can grip the fetal head with. If all five fingers can grip the fetal head just above the mother's pubic bone, the head is not yet engaged.
As you learned earlier in this session, there are important terms for measuring uterine contraction:
Measuring uterine contraction:
- The frequency of the contraction (how many contractions per ten minute
- The intensity of contraction ( how painful her contraction is)
- Duration (How long each contraction of uterus lasts/onset to peak)- contraction lasts stronger
Auscultation:
You can appreciate fetal heartbeat by fetoscope or stethoscope on maternal abdomen between contractions, preferably at the side of the abdomen where the fetal back is located. Normal fetal heart beats ranges from 110-180 beat/minute. Any rate below 120 beats/ minute and above180 beat/minute indicate fetal distress, and you should refer unless the labour is progressing fast and the fetus is about to born.
Vaginal examination:
Careful vaginal examination gives a lot of information. Always, do a vaginal examination every 4 hours. It would help you to:
- To diagnose the position and presentation.
- To know whether true labour started since its contraction results in cervical dilation.
- To know the station about ischial spines.
- To check cord prolapsed after the membrane is ruptured.
Make sure you take care to avoid introduction of infection into the sterile uterus especially if the membrane is broken.