Privacy and confidentiality
The professional relationship between a health professional and a client in a rural community is frequently long-term, and may involve the wider families and mutual friends. This closeness may well affect professional responsibilities. In this section you will study the ethical conflicts involving privacy and confidentiality in rural healthcare relationships. Confidentiality may involve more complex issues in rural rather than urban settings. People who live in rural areas may well know many of the details of each other's lives and this intimacy makes ethical conflicts related to privacy and confidentiality more challenging compared to urban settings.

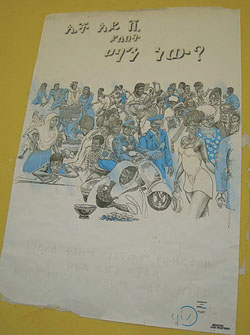
Case Study: Confidentiality and trust
Ali has been a soldier for the last five years. He's now returned to his rural village and started to help his father on their farm. He's a strong and handsome man and soon starts to see a new girlfriend Kedija. Ali comes to the health facility and shows the health professional, Workinesh, the results of his recent HIV test – which is positive. Workinesh also has information through her work that neither Kedija nor Ali have asked for, or been given any, condoms. What should Workinesh do?
Almost anything that Workinesh does actively will risk breaking confidentiality. But doing nothing will potentially harm one of her patients, Kedija. If she doesn't warn Kedija that Ali is HIV positive then Kedija might become infected and become seriously ill and even die. Several ethical principles are at stake here including trust, confidentiality and autonomy. Nobody can force Kedija or Ali to act in a particular way because they each have their own autonomy.
Which of the following actions do you think that it would be ethical and appropriate for the health professional to do? Explain your reasons.
- Do nothing and hope that her patient Kedija doesn't get infected.
- Make sure that Ali is aware of his responsibilities and also offer him condoms.
- Go round to Kedija's house and tell her that Ali is HIV positive and that she should use condoms.
- Ask for help from an experienced healthworker at the hospital or higher health facility.
Although answer d. is appropriate in this case and Workinesh should always seek appropriate support and assistance in difficult matters, perhaps she can also use her ethical principles to help her decide what else to do. Answer a. is not appropriate ethically. This course of action risks harming her patient. If she does make sure that Ali is made aware of his responsibilities (answer b.), and that he will always use condoms in the future, then she has followed ethical principles and protected her patients to the best of her abilities. Answer c. is probably only possible ethically if she also does b. To tell Kedija the test results of her partner is not ethically acceptable unless this is cleared by the person who has been tested.